Summary Care Record (SCR)
Published on: 10th May 2016 | Updated on: 2nd February 2024
 The NHS Summary Care Record (SCR) is an electronic summary of key clinical information (including medicines, allergies and adverse reactions) about a patient, sourced from the GP record.
The NHS Summary Care Record (SCR) is an electronic summary of key clinical information (including medicines, allergies and adverse reactions) about a patient, sourced from the GP record.
It is used by authorised healthcare professionals to support their care and treatment. More than 96% of the population have an SCR because they have not opted out and it is already being successfully used in many settings across the NHS, such as A&E departments, hospital pharmacies, NHS 111 and GP out of hours services and walk in centres. The SCR differs from Shared Care Records (ShCR); ShCRs include additional information and from additional settings.
The SCRa application portal is being replaced by the National Care Records Service (NCRS) portal during 2023. From now until around Autumn 2023, both the SCRa portal and the NCRS portal are expected to be accessible.
The National Care Records Service (NCRS) is being introduced as a new interface available from within the Spine portal link directory to provide national patient information for health and care staff with NHS Smartcards or equivalent. NCRS will be a successor to the Summary Care Record application (SCRa) portal.
NCRS enables view of SCR information but additionally view of:
- Personal Demographics Service
- National Record Locator (NRL)
- Locally held care plans can also be included
- Reasonable Adjustments Flag (RAF)
Information within NCRS is consumable by IT system suppliers. Some items within NCRS can be amended by health care staff, for example the RAF.
Authorised health and care professionals can access the National Care Records Service using mobile or desktop device connected to the internet using WiFi, mobile data or an existing Health and Social Care Network (HSCN) connection. The NCRS offers multiple access options including biometric authentication or smartcards. The NCRS is being piloted in different health and care settings including within Weldricks pharmacies, and wider roll-out is anticipated.
Try out NCRS now: Pharmacy professionals are encouraged to test out NCRS by going to: https://portal.spineservices.nhs.uk/nationalcarerecordsservice/ (on their Patient Medical Record (PMR) machines with their Smartcard) and dummy test patient NHS numbers are available to allow practice/training 999 040 2132, 999 025 2955 and 999 024 0272. Professionals that have tested NCRS can complete this 3-minute CP ITG NCRS feedback snap survey (or email it@cpe.org.uk).
Read more: NCRS
For information about SCR and multi-site arrangements please refer to the briefing at: cpe.org.uk/scmultisite.
Before and during the start of the COVID-19 2020 pandemic, Community Pharmacy England supported NHS Digital’s work to look at adjusting the flexibility of Smartcards whilst maintaining integrity of the Smartcard system. Developments during 2020 included:
- NHS Digital confirmed their position regarding RA flexibility “Wider use of National Locum Pharmacy Agency code and position (FFFFF) can be used. It is important that RAs keep a log of users given this access for exceptional reasons so that it can be revoked as appropriate at some point in the future.” (24th March 2020 NHS Digital website).
- Those pharmacy team members with the pharmacist and 5F codes on their card were granted SCR rights associated with the 5F code for at least one year. This bulk adjustment performed by NHS Digital meant that if the staff used the 5F at various pharmacy premises, they could still access SCR information. A new card role, “National Locum Pharmacist + SCR – COVID-19”, was added to smartcards from late April 2020. The new Smartcard code is planned to automatically expire after one year. This activity was performed centrally so that no action should have been required by pharmacy team members or local RAs.” (From April 2020).
- RAs have been encouraged to be aware that provisionally registered pharmacists can have access to SCR of the using the ‘National Locum Pharmacist + SCR – Covid19’ position for a period of 12 months. This is recognising that newly qualified pharmacists are experiencing delays converting from pre-registered to fully registered with the General Pharmaceutical Council (GPhC) because they are unable to sit assessments with the GPhC. NHS Digital is helping to progress these applications and has issued guidance for RAs.
Read about updating Smartcards and applying the SCR code if you still need to at: Updating Smartcard roles.
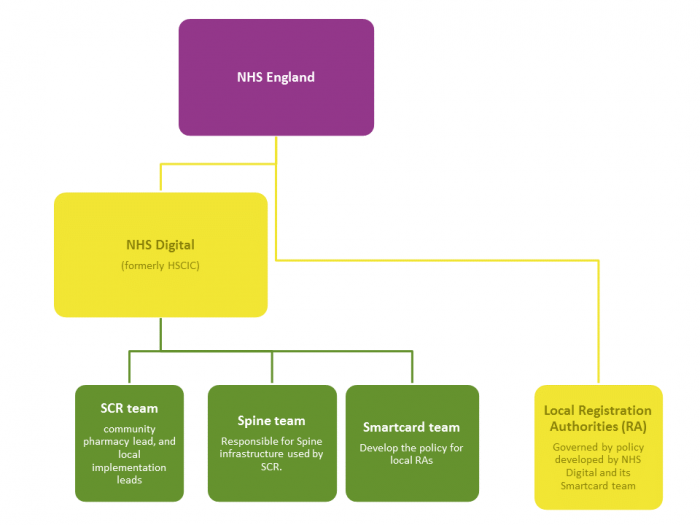
NHS England and NHS Improvement through its local teams is responsible for the issue of Smartcards and commissions local Registration Authorities (RAs) to carry out this function.
Contractors should report any concerns about the adequacy of local RA arrangements to LPCs. LPCs can use the escalation process which sets out LPCs may raise concerns directly to Community Pharmacy England’s IT team (it@cpe.org.uk).
The NHS Digital central Smartcard team issue policy and guidance for use by the RAs.
Overview
More than 96% of the English population are part of the Summary Care Record (SCR) initiative – with less than 4% opting out.
Standard SCR displays some standard information. SCR with Additional Information includes richer information so that health and care workers can provide enhanced care.
Framework for use (during the COVID-19 pandemic)
In light of the current emergency, the ‘Additional Information’ framework was amended from April 2020 so that health and care workers that can use SCR can view the information best needed to support patients including Additional Information. For the time being patients will not have to ask their GP practice to activate it. This arrangement will be reviewed after the pandemic.
Framework for use (before the COVID-19 pandemic)
Patients confirm their consent by requesting that their GP practice activates SCR with AI for them so that other health and care workers such as their pharmacist may have ability to have sight of that information when needed.
Patients request to their GP practice that the practice enables SCR with Additional Information for them.
A small but growing percentage of patients (around 5% of patients so far) had actively requested their GP practice activate SCR with Additional Information so that pharmacy staff and others can access more information where needed.
Additional information can only be included with the patient’s consent, unless they don’t have capacity to consent. The GP practice activate SCR with Additional Information on a patient-by-patient basis. Additional information may, on occasion, also be added to the SCR of a patient who lacks capacity to consent where the GP makes a relevant determination.
Comparing standard SCR to SCR with Additional Information
Read Community Pharmacy England’s Comparing standard SCR to SCR with Additional Information factsheet to learn of the differences. See also below:
| Standard SCR | SCR (Additional Information) | Excluded from standard SCR and SCR with Additional Information (by default) |
| • medicines; • allergies; • adverse reactions; • Shielded Patient Flag |
Additional information can include any or all of these: • reason for medication; immunisations; • significant diagnoses / problems; significant procedures; • end of life care information and patient preferences; • other anticipatory care preferences, when they have been recorded by the GP; and • other important information from the GP record that the patient and GP agree should be included in the SCR. |
There are items which are excluded from both SCR types unless the patient specifically asks for these to be included: • fertility treatment; • sexually transmitted infections and treatments; • terminations; and • gender reassignment. |
Local campaigns
Within some areas, local stakeholders may support campaigns for patients and health and care workers to be able to make greater use of SCR with Additional Information and be aware of its benefits.
Pharmacy teams and LPCs are encouraged to support any local or national campaigns that promote SCR with Additional Information.
Resources for patients about SCR with AI
NHS Digital resources include:
- Consent form for SCR with AI
- Consent form for patients new to a GP practice
- Printable poster (designed for display within GP surgeries)
- SCR with AI patient leaflet
- Easy read format patient leaflet about SCR with AI
Survey findings: SCR with AI
NHS Digital published survey results indicating that 71% of clinician respondents that accessed SCR Additional Information to support patient care, said that viewing additional information helped make more effective use of time with patients due to:
- less need for time finding information;
- reduced number of calls to GP Practices or other health and care organisations;
- the information supporting decision-making; and
- avoidance of referral to another health care provider.
Patients sharing additional information explained within their survey results that one of biggest reasons they decided to enable sharing of additional information was so that health and care workers would be able to understand “why I take a particular medicine”.
Pharmacy usage of SCR and SCR with AI
Pharmacy teams are encouraged to make use of SCR and SCR with Additional Information (where available) to enhance the care they can provide for their patients e.g. when delivering a service or providing emergency supply. Increasingly patients will also be able to access health information with the NHS App if GP practices have enabled NHS App features.
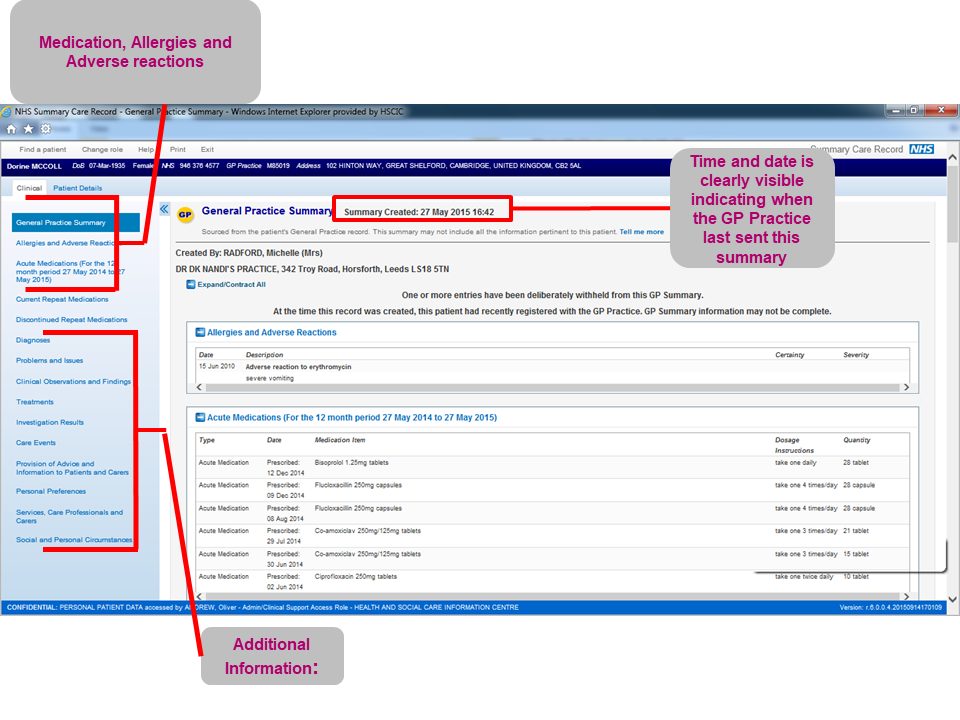
A screenshot example of SCR with Additional Information can be seen below:
See also:
Core information within SCR
The core information automatically included within SCR is:
- all known allergies & adverse reactions recorded for that patient on the GP system; and
- all medications within the following conditions:
- Acute medications (6 or 12 months depending on the GP system);
- Current repeat medications (with last issue date dependent upon GP system); and
- Discontinued repeat medication (if the GP system adds this data, 6 months).
Additional Information within SCR
Patients may request to their GP practice that the practice adds other useful content beyond the core data set. If this data has been added to the appropriate record field by the GP practice, then the person accessing SCR will be able to view:
- reason for medication;
- immunisations;
- significant diagnoses / problems;
- significant procedures;
- end of Life Care information and patient preferences;
- other anticipatory care preferences, when they have been recorded by the GP; and
- any other important information from the GP record that the patient and GP agree should be included in the SCR.
There are items which are not included unless the patient specifically asks for them to be. These are details of:
- fertility treatment;
- sexually transmitted infections and treatments;
- terminations; and
- gender reassignment.
SCR access checklist
The process for community pharmacy contractors and pharmacists and pharmacy technicians to use SCR is set out at the SCR checklist. That also applies to a newly opened pharmacy which will have relevant staff use SCR.
SCR webinars hosted by Community Pharmacy England/NPA
Make sure you watch two related webinars to find out how to get the most out of Summary Care Record (SCR) access in your pharmacy.
The first webinar, hosted by Community Pharmacy England and NHS Digital is available on-demand. It covered getting ready, the benefits of SCR usage, how to use SCR to improve efficiency, and top tips and experiences from users. The second webinar, hosted by the National Pharmacy Association (NPA), is also available on-demand here.
NHS Digital explained how SCR can help improve the day to day running of a pharmacy and shared examples of life-saving interventions that could not have happened without it.
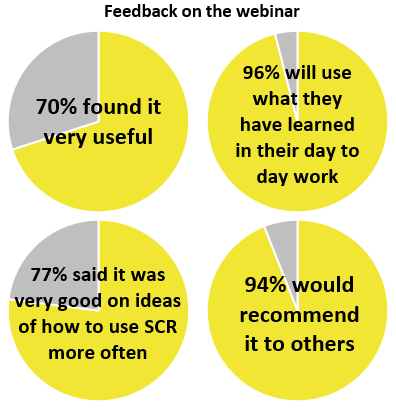 Following the presentation and a video interview with Pharmacy Manager Shaheen of P&S Chemist Ltd, Community Pharmacy England’s Dan Ah-Thion chaired an informative question and answer session covering a range of questions from who can have access to scenarios when it could be used.
Following the presentation and a video interview with Pharmacy Manager Shaheen of P&S Chemist Ltd, Community Pharmacy England’s Dan Ah-Thion chaired an informative question and answer session covering a range of questions from who can have access to scenarios when it could be used.
An on-demand recording of the webinar is available to watch at: cpe.org.uk/SCRwebinar. To view the recording, you will need to register (or input the email address you registered with previously).
Part 1 feedback included:
- “After this webinar I feel more confident about using SCR. I haven’t done face to face training but I look forward to doing it and I am not scared of using SCR in my busy day to day work.” -Pharmacy Manager
- “Brilliant and very informative. The FAQs were really useful and answered very professionally from someone who really knew every aspect of SCR.” – Pharmacy Owner
- “Best webinar yet with lots of really useful information.” – LPC Member
| Title | Date and time | Host |
| SCR Part 1: Getting started and using efficiently | On-demand | Community Pharmacy England |
| SCR Part 2: Privacy and liability |
On-demand | NPA |
If you’re not yet SCR-live then, before watching these webinars, please review the SCR checklist, and of course you will still need to attend a face-to-face implementation briefing event (see below).
Note: Before April 2016 face-to-face training was necessary but this is no longer required.
CPPE online training
All pharmacists and pharmacy technicians who will access the SCR must have completed the Centre for Pharmacy Postgraduate Education online SCR training and assessment module prior to accessing the SCR.
The Centre for Pharmacy Postgraduate Education (CPPE) has also launched an e-learning programme on the use of Summary Care Records in community pharmacy intended for pharmacists, pharmacy technicians and pre-registration trainees who are about to begin using the SCR. Whilst this can be completed at any time (and provides excellent information on SCR in general), the best time for it to be completed is close to the time when your pharmacy will be going live and starting to access to SCR e.g. just before attending the face-to face event so that SCR can begin to be used immediately following the event.
Once you have completed the e-assessment, you can tick the box under the ‘Summary Care Records assessment registration process’ heading in your profile on the My CPPE section of the website. This will allow the Registration Authority (on behalf of NHS Digital) to see that you have passed the assessment and then allow you access to SCRs on your Smartcard.
SCR Governance Person (previously called ‘Privacy Officer’) training
See the ‘SCR Governance Person’ section of this webpage.
Using NHS Digital’s portal application
Logging on and searching test or real patients
Launch the NHS Spine portal: https://portal.national.ncrs.nhs.uk/portal/ (Smartcard required) and select ‘Launch SCR’ and start using SCR.
To practise and test usage: enter test example (dummy) patient numbers such as: 999 040 2132; 999 025 2947; 999 025 2955; 999 024 3271; or 999 024 0272.
Practising helps staff for when real usage is needed.
NHS Digital have published leaflets to assist pharmacies:
- Logging on and searching for a patient (GemAuthenticate)
- Logging on and searching for a patient (Identity Agent 2)
NHS number is used where known, some pharmacy teams obtain this using their EPS module or PMR, and paste this into the SCR application.
When to use SCR
Pharmacy teams report that the SCR can be used as an alternative to contacting the GP practice in some scenarios.
SCR may also be used by contractors who do not currently have access to more detailed electronic health record systems such as their Local Health and Care Record (LHCR) system. LHCR records include more information from the GP record compared to SCR.
SCR medicines information may also be provided within the existing pharmacy clinical system if the pharmacy supplier has added this type of integration.
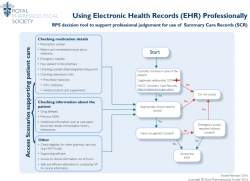
The Royal Pharmaceutical Society (RPS) has published a one-page factsheet which explains those scenarios in which to use the SCR or another electronic health record (e.g. the LHCR if you have access to it). The decision as to when to use SCR or another electronic health record is a professional one.
Listed scenarios
Checking medication details
• Prescription unclear
• Patient can’t remember/unsure about medicines
• Emergency supplies
• New patient to the pharmacy
• Checking possible dispensing/prescribing error
• Checking interactions with:
• Prescribed medicines
• OTC medicines
• Herbal products and supplements
Checking information about the patient
• Drug allergies
• Previous ADRs
• ‘Additional information’ such as care plans/blood test results, immunisation history, intolerances
Other:
Check eligibility for other pharmacy services (e.g. NHS flu jab)
• Supporting self-care
• Access to clinical information out of hours
• Safe and efficient alternative to contacting GP for clinical information
FAQs: Using SCR
Q. Will SCR allow me to check whether a prescription is eRD?
A. The EPS Tracker allows this functionality, but the SCR currently does not. In some scenarios Tracker and SCR are used together in unison.
Q. Will locums using SCR have their accesses associated with our pharmacy?
A. Pharmacy staff which have Smartcards with only the FFFFF multi-site code, and SCR usage rights associated with their FFFFF general code, will be asked to select which pharmacy they are working in. The SCR usage will be counted as an SCR access for the selected site.
Q. Are pre-registration pharmacists and pharmacy technicians able to access SCR?
A. No. Two agreed professionals regulated by General Pharmaceutical Council (GPhC) can access SCR: pharmacists and pharmacy technicians.
Pre-registration trainees can do the Centre for Pharmacy Postgraduate Education (CPPE) training in preparation for qualification. The suggestion is that trainees do this close to the time that they are to qualify so that the learning is maximised.
System suppliers can integrate the use of SCR information so that SCR information can be accessed more quickly and easily for when required.
Accessing SCR information
The SCR might be accessed in different ways such as:
- The standalone web viewer SCR application (known as the SCRa): This does not require any additional software.
- Integrated viewer: May be developed by system suppliers to allow users to view the SCR within their existing clinical system.
- 1-click functionality developed by system suppliers for their system/s (available via Lorenzo (CSC) or Servelec RiO)
- orQestra® SCR Spine Mini-Service Provider (Quicksilva): can be integrated with any of the pharmacy PMR systems with their support.
SCR 1-click available within Sonar and PharmOutcomes from 2019
Pharmacists and technicians can access vital patient information quickly through the Summary Care Record (SCR) 1-click feature that is available within the PharmOutcomes and Sonar systems.
The 1-click function allows pharmacy professionals logged in with their Smartcard to click straight through to a selected patient’s SCR whilst using PharmOutcomes or Sonar, without having to log in separately and complete a manual search by entering an NHS number.
This can help SCR to be used as part of providing pharmacy services such as NUMSAS and the Digital Minor Illness Referral Service.
Having access to a patient’s Summary Care Record speeds up care and reduces the need for phone calls to GP practices, delays to care and the need for referrals to other services, particularly out-of-hours.
Community Pharmacy England and the Community Pharmacy IT Group have encouraged all PMR suppliers to similarly implement SCR 1-click functionality into their software.
Learn more at: the PharmOutcomes SCR 1-click video guide. Visit the Sonar Informatics website for more information about their system.
System suppliers and SCR/NCRS
EPS and Community Pharmacy Contractual Framework (CPCF) system suppliers or system users may inform Community Pharmacy England about progress:
| System | System supplier | SCR integration or SCR 1-click feature present | NCRS 1-click |
| Analyst | Positive Solutions | Rolling out | Not yet rolled out. Delivery plan to be confirmed. |
| CoMPass / LS | Lloydspharmacy | tbc | tbc |
| Nexphase | Cegedim Rx | tbc | tbc |
| Pharmacy Manager | Cegedim Rx | Rolling out | tbc |
| PharmOutcomes | Pinnacle Health LLP | 1-click feature present for certain service modules | Work planning to be scheduled in for for NHS Q1 ready for completion for Q2. |
| ProScript systems | EMIS | tbc | tbc |
| ProScript LINK | AAH Pharmaceuticals | tbc | tbc |
| RxWeb | Clanwilliam Health | tbc | tbc |
| Sonar | Sonar | 1-click feature present for certain service modules | Currently scheduled to go live with after being accredited in Mid 2022 |
System Supplier status updates: If you are a pharmacy system supplier that is developing or currently supplying an SCR enabled PMR System to the English market and would like your name added to this list please contact Community Pharmacy England. If you are aware that details above have changed please let us know. EPS and CPCF IT Suppliers needing to speak with NHS England about integration options may contact Summary Care Record (SCR) and NHSE TD live services team: liveservices.operations@nhs.net.
The consent framework was established during 2017 when pharmacy teams began to make use of SCR and was agreed by NHS Digital, Community Pharmacy England and others at that time as a starting point consent model. The framework may be updated later as SCR usage becomes more common.
Consent framework
Each patient should provide for you their “permission to view” (PTV) before you access their SCR.*
*Unless the “Accessing SCR without a patient’s consent” method is being used – see section below
The key information to pass on when obtaining consent is:
- What SCR is: Some contractors explain it includes ‘information from within the GP practice record’.
- Why the pharmacy will access their record e.g. ‘to support your care’.
- How often will the pharmacy access? You can ask for a one-time access or could ask them for permission to view their SCR while they are in your care. If long-time access is granted you could put a note in the patient’s PMR (e.g. ‘consent given for ongoing SCR access’).
- PTV can be withdrawn by the patient: The patient should also be informed that they can change their decision at any time.
Verbal confirmation is generally the best way to obatin consent, although some contractors may opt for written confirmation (especially where the permission is ongoing). There is a sample form for recording this further below.
Opting out of having an SCR
All patients in England have been communicated to with regards to having an SCR; they have the ability to opt-in or opt-out at any time. If a patient wishes to opt-out of having an SCR altogether (as opposed to just not letting you view it) then they should be advised to contact their GP practice who will record this preference.
Accessing SCR without a patient’s consent (emergency access)
The ‘Emergency Access’ option can be used if a patient or the person acting on their behalf is not able to give their consent, but you believe there is still a clinical requirement to view their SCR.
In this instance you should use professional judgement and if you decide that accessing the SCR is necessary and in the patient’s best interests (i.e. there is a possibility that without accessing the patient’s SCR the quality or safety of the decision would be compromised), then you should use ‘emergency access.’
As with any professional decision you need to be confident that you can justify to any future investigation that the decision was made in the patient’s best interests. Whenever the “Emergency Access” option is selected it is strongly recommended that you enter the reason why you are accessing the record without the patient’s permission. This will assist the work of the SCR Governance Person (see relevant section of this webpage) investigating the legitimacy of emergency accesses.
Examples of when this option could be seen as appropriate in community pharmacy are:
- a patient with language difficulties; or
- elderly patients with dementia.
See also, the GPhC guidance on consent which mentions: “If the patient is not able to make decisions for themselves, you must work with people close to them and with other members of the healthcare team.”
SCRs for children
Children can have an SCR, and in instances where the child understands what is being asked of them,
permission to access SCR is their decision. If the child does not understand then it is the parent or guardian’s choice. This is at the Pharmacy professional’s discretion. Refer to GPhC guidance on consent.
Patient consent form templates
Consent is often best to obtain verbally because in many case pharmacy teams report that patient already have access to this information to support their dispensing work. However, there is a template:
NHS Digital sample form (PDF)
FAQs about SCR consent model
Q. My pharmacy serves a large care home. How can the patients provide their consent to SCR access or could this be done by care home staff?
A. Community Pharmacy provides services to patients in care homes, mostly without communication with the patient; with the care home requesting services for patients ‘by proxy’. The RPS advise that the process for obtaining consent to be used is for:
- The care home informs patients/their carers upon arrival that their preferred pharmacy may access SCR. This could be added to admission forms. The patient/carer must inform the care home if they do not give their permission for the SCR to be accessed.
- Patient information, leaflets and posters should be made available at the care home – examples can be found on the patient materials (SCR) page.This is required to meet Data Protection Act rules on fair processing.
- The pharmacy and care home have an understanding where any patient/carer refuses permission, they will inform the pharmacy NOT to access SCR. Otherwise, the pharmacy can access SCR based on the above.
- If the patient has not completed the arrival process, then care home can give permission by proxy, as appropriate.
Q. What if I believe that accessing the SCR for a Care Home patient is needed, but I cannot obtain consent?
A. There is a consent model as explained above. In emergency situations where this model is not applicable, pharmacy may consider emergency access (described earlier).
Q. How long should I keep an SCR consent form that has been signed by the patient?
A. Pharmacies must have processes for obtaining explicit consent from the patient or their representative before accessing a patient’s SCR. This may involve SOPs. Written consent is not required but it can be obtained. It is for a contractor to judge how long forms should be kept for, balancing the need for an audit trail against the fifth Data Protection principle of not keeping information longer than necessary.
Q. If I am obtaining SCR consent in writing, can I ‘bundle’ together the request for SCR consent, with the consent being requested for another activity?
A. Obtaining informed consent is required and therefore we do not recommend that SCR consent be ‘bundled’ with another written request for consent, if this could risk the patient not noticing that they may have ‘granted’ consent for SCR accesses. One way to avoid unintentional ‘bundling’ of a request for SCR consent, is for a separate ‘tick’ (or an equivalent) on a written form or equivalent. Obtaining informed consent is necessary.
SCR usage is encouraged where the pharmacist or technician determines it useful and with consent where required. A person for each pharmacy will be able to view alerts about SCR activity, and take action to investigate only where needed. This person is called the ‘Governance Person’ (SCRGP), previously known as ‘Privacy Officer’. Read more below if you will be carrying out this role or assigning it persons within your pharmacy.
Who will access SCR and when?
Once a pharmacy has become ‘SCR live’, SCRs will only be accessed within that pharmacy:
- by pharmacists and pharmacy technicians;
- once the SCR requirements have been fulfilled;
- when the patient has provided their consent and permission to view (PTV) or in an emergency scenario; and
- where there is a legitimate relationship (LR) with the patient i.e. the pharmacy team are involved in the patient’s care at that point in time.
What measures are taken to protect patient data?
Security measures include:
- Smartcard users have agreed to use their cards in line with the user policy;
- Standard Operating Procedures (SOPs) for SCR use must be in place;
- the professional code of conduct, and employment contracts must be adhered to; and
- contractors complete the Data security and Protection Toolkit each year.
How are SCR accesses auditable?
- Every SCR-access is fully auditable and linked with the Smartcard ‘logged in’ at that time.
- Privacy alerts are generated by accessing SCR. These also indicate when the emergency access option is used.
- Reports are available to show every record accessed by every Smartcard.
- Patients can request to see who has accessed their SCR at any time.
Who will audit SCR access?
Each pharmacy organisation that has access to SCR must have a nominated person who is responsible for monitoring the SCR usage of the pharmacy’s SCR users – the SCRGP.
This person will audit SCR accesses and manage privacy alerts.
How will the SCRGP audit SCR access?
Privacy alert notifications (if you have NHSmail) can provide prompts for the SCRGP to investigate SCR access and to check that the accesses have been appropriate. Use of the Alert Viewer tool is also an option.
The SCRGP will review the pattern of privacy alerts at regular intervals to spot anomalies.
Example scenarios in which the SCRGPs may investigate include:
- an unexpectedly high number of emergency accesses;
- recurring access to the same patient’s SCR;
- access during closing hours;
- no record of the reason for access;
- apparent access by a branch before it has gone live with SCR;
- disproportionate accesses being made by one member of staff; or
- unusual patterns are spotted.
Where the access is legitimate than the privacy alert is closed and no further action is required.
In the event that any illegitimate access is confirmed during the investigative process, local guidelines will apply. The ‘Care Record Guarantee’ document says that: “If we find that someone has deliberately accessed records about you without permission or good reason, we will tell you and take action. This can include disciplinary action, which could include ending a contract, firing an employee or bringing criminal charges.”
Glossary
SCRGP = Governance Person in regards to SCR. Older documention refers to ‘Privacy Officer’, but this has been re-described to better describe the role.
FAQs: SCRGP
Q. I have accessed the NHS Digital’s ‘SCRa’ portal demographics screen of a patient to check whether a patient has the Shielded Patient Flag, will this generate a privacy alert?
Community Pharmacy England have been advised by NHS England and NHS Improvement that access to the demographics screen of the NHS Digital’s ‘SCRa’ portal will not generate a privacy alert.
Q. How many SCRGPs need to be appointed?
A. The number of individuals undertaking the role of the SCRGP will vary amongst different community pharmacy organisations. Organisations may take into account the frequency of usage, number of staff accessing, and the number of branches live with SCR, when assigning the SCRGP role(s). SCRGPs are responsible for checking appropriate use across the organisation.
Q. How much time is required to undertake the SCRGP role? How many alerts require checking?
A. There is no mandated number of privacy alerts which require investigation. Initially some pharmacies may decide to check around 10% of privacy alerts each month, although this will depend on the circumstances of the pharmacy, the total number of SCRs being accessed, and the trends being identified. One pharmacy team may decide to take a few minutes each week for checks, another pharmacy team may use more time, but check each quarter. The regularity of the checks may be reviewed and adjusted as processes become embedded into practice, or in the event of evidence of inappropriate usage.
Q. Who can be a SCRGP in community pharmacy?
A. Every pharmacy has a nominated SCRGP prior to accessing SCRCR. It is useful for at least two people to have SCRGP role – a primary SCRGP, and somebody to cover for sick/annual leave. The designated SCRGPs ideally should not have access to SCR for the pharmacy branch they work in. However, this may not be feasible in small pharmacies, and pharmacy professionals with access to SCR may also have the SCRGP role. In this setting, the support SCRGP will monitor the primary SCRGP’s access and vice versa.
Read more at: SCRGP guidance, user guides and training materials (NHS Digital).
The pharmacy privacy notice may explain that pharmacy professionals will access records such as SCR and Shared Care Records.
“Our pharmacy professionals may consult relevant records to support your care, such as NHS summary care records or local shared care records. We align with NHS protocols for use of records. We may also ask you if, whilst you remain under our care, our pharmacy professionals can consult relevant records. If you allow us to see those health records this will help to ensure that relevant medical information is visible to our professionals.”
A template privacy notice can be found at: cpe.org.uk/dstemplates.
For locally produced SCR communication materials, pharmacies need to take care to ensure compliance with the NHS Brand guidelines if planning to use the NHS logo.
Increasingly patients will also be able to access SCR and other health information (e.g. from their Shared Care Record) within the NHS App, if GP practices have enabled NHS App features.
Pharmacy contractors: general SCR statistics
NHS Digital SCR stats pages:
- SCR stats links
- SCR weekly stats page (with downloadable spreadsheets available each week)
NHS Digital PowerBI dashboards:
Quality Payments: SCR calculator available
NHS Digital’s Summary Care Record (SCR) calculator webpage, for Quality Payments Schemes. To use the calculator:
- access the dashboard data;
- use the arrows at the bottom to scroll between weekly SCR views and the QP calculator;
- enter your pharmacy name or ODS (F) code into the search box;
- select from the list, or scroll through the pharmacy list to select; and
- view totals in the box (correct as of the date the data was extracted).
The SCR calculator does not provide live information; it is only updated weekly on Thursdays (with the previous week’s viewing figures as of the end of Sunday). The calculator states the date of the data being used. SCR usage data in raw spreadsheet format will continue to be published for those that need to use this spreadsheet data for their bespoke analysis.
NHS Digital are also publishing the data in spreadsheet format on their calculator webpage.
Local Pharmaceutical Committee (LPCs) SCR statistics
Pharmacy level SCR statistics by LPC area (2MB excel spreadsheet)
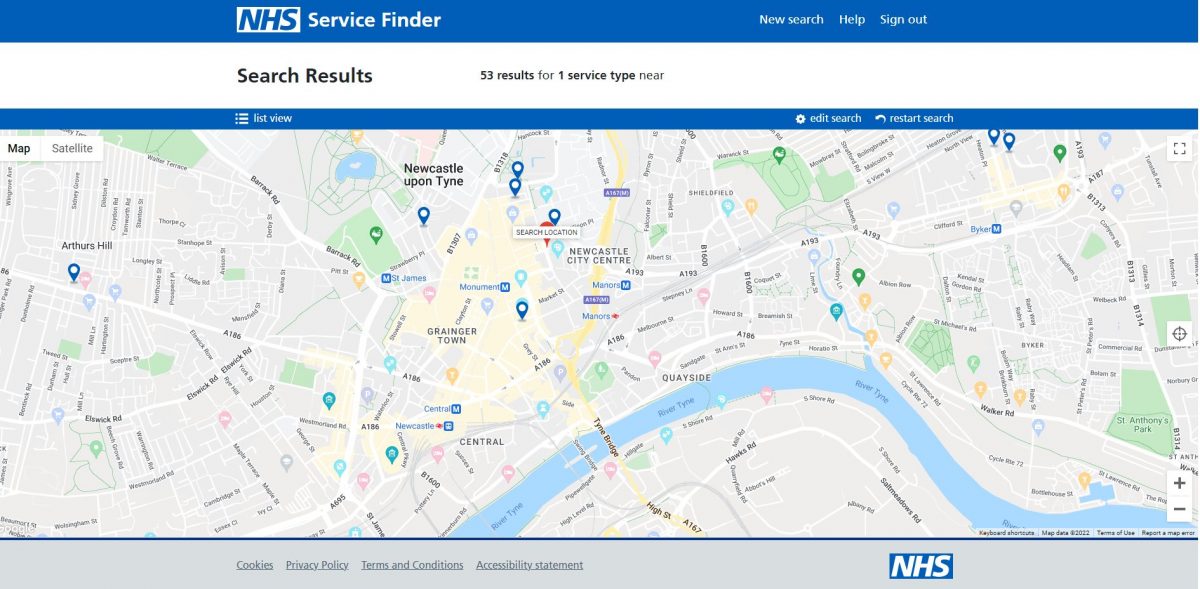
Interactive map of live pharmacy sites
NHS Digital update a live map of those community pharmacies which have gone live with SCR.
You can zoom into your area to check which pharmacies have already gone live in your area:
A number of organisations and people are involved with the implementation and technical oversight of the SCR.
NHS Digital
NHS Digital manage the national infrastructure for a variety of NHS IT projects including the SCR.
NHS IT Operating Model
NHS England are responsible for undertaking a range of tasks that support pharmacies in accessing and using national NHS IT applications.
The document, “Securing excellence in IT Services” set out NHS organisational responsibilities in relation to IT. NHS England, through its local teams may either provide support functions itself or make arrangements for commissioning support units (CSUs) or any other IT provider to deliver them.
GP IT services will be managed by clinical commissioning groups (CCGs) on behalf of NHS England. A CCG may choose to provide support functions to GP practices itself or make arrangements to commission support from CSUs or another IT provider – whilst it is possible that in some areas, NHS England and CCGs will commission the same CSU to provide SCR support for pharmacies and GPs respectively, this may not always be the case.
SCR business continuity and feeding back about SCR issues
When SCR is down, or there is a failure with Smartcard access then an alternative to its use is contact with the GP practice as would have been the case prior to the pharmacy being live with SCR.
Sign-up to receive Spine alerts so that you will be notified if NHS IT components fail which prevent SCR access. For more on SCR and NHS IT business continuity issues read here.
Depending on the nature of any technical difficulty, you may wish to contact:
- your local project contact;
- your usual IT helpdesk; or
- the national SCR programme
Community Pharmacy England recommends pharmacy staff use NHS IT business continuity tools such as:
| System Alerts: Staff can register to receive text or email alerts in the event that the national NHS Digital systems that support SCR are experiencing issues at Spine alerts. | |
| Checker: Visit the NHS Digital service status checker webpage which provides information about the status of the national systems at EPS checker. |
Note that system Spine alerts differ to SCR privacy alerts.
Pharmacy team members may also contact Community Pharmacy England: it@cpe.org.uk to comment on a technical issue being escalated to NHS Digital or to feedback about the SCR.
Tips include:
- SCR web address added to favourites – The pharmacy team may choose to add the SCR URL to desktop/favourites to make future access quick and easy.
- Patient information – The pharmacy team may choose to make patient information materials (posters, leaflets) available at the pharmacy and on the pharmacy website (see here).
- Standard operating procedure (SOP) in place – The pharmacy team need an SCR SOP. A template is available here SCR access could also be integrated into other SOPs.
SCR views from pharmacy / pharmacist
P&S Chemist clip from the full webinar:
Clip from the full webinar about scope for regular usage:
COVID-19 SCR-related changes
- COVID-19 codes: COVID 19 SNOMED codes were added to the Summary Care Record Additional Information dataset
- SCR with Additional Information: In light of the current emergency, the ‘Additional Information’ framework was amended on 23rd April 2020 so that health and care workers that can use SCR can view the information best needed to support patients – including ‘Additional Information’ (e.g. diagnoses information). This means for the time being patients won’t need to ask their GP practice to activate it. This arrangement will be reviewed after the pandemic. Pharmacy teams are encouraged to email it@cpe.org.uk if they wish to share evidence about how the change helps aside from the pandemic, to support review of whether the arrangement will continue.
- Smartcard & multi-sites process: Community Pharmacy England has supported NHS Digital’s bulk adjustment of cards with the locum 5F code to be associated with 5F SCR code.
COVID 19 SNOMED CT (Systematized Nomenclature of Medicine — Clinical Terms) were added to SCR Additional Information dataset to capture suspected or confirmed COVID 19 status from GP systems.
If GP practices use these codes on their clinical systems, this should feed across into SCR Additional Information.
Read more at: NHS Digital website.
Currently, only the patient’s GP practice can add information to the SCR.
For more about ‘writing’ to records see: Write access to Electronic Health Records.
NHS Digital have previously said they will welcome ideas relating to Smartcards or access control which are:
- good value to those who pay for it;
- work for the people who use it; and
- feasible to deliver with the resources available.
For instance one of the projects being looked at includes exploring giving more health and care workers quick and secure access to healthcare information and systems from tablets and mobile devices with and without Smartcards.
They also appreciate feedback regarding the Care Identity Service.
To submit ideas email cisuat@nhs.net. Please cc Community Pharmacy England: it@cpe.org.uk.
Regulatory matters: use of SCR
From 1 April 2016, the terms of service began to require NHS pharmacists who have access to SCR to access this if they consider, in their clinical judgment that it is in the best interests of the patient to do so.
If an NHS pharmacist does access the SCR then this must be in accordance with The NHS Care Record Guarantee guidance.
Community Pharmacy England is sometimes asked whether contractors must access SCR and when. Community Pharmacy England’s position is that if you have access to SCR and consider in your clinical judgment that it is in the best interests of the patient to access SCR then you must do so. If so, then your access of SCR must be in accordance with The NHS Care Record Guarantee guidance available here.
Pharmacy contractors with access to more detailed records such as Local Health and Carer Records (LHCRs) may make a determination that access to the LHCR means an additional access to SCR would not be necessary.
Regulatory matters: consistent access to SCR
From 9th November 2020, pharmacy contractors must ensure that staff working at their pharmacy can access NHS Summary Care Records (SCR) and that access is consistent and reliable during the pharmacy’s opening hours, in so far as that is within the control of the contractor.
SCRs can only be accessed by pharmacists and pharmacy technicians, and this regulatory change does not amend that. Subject to the normal patient consent requirements, those registered professionals should access patients’ SCRs whenever providing pharmaceutical services to the extent that they consider, in their clinical judgement, that it is appropriate to do so.
Most contractors have previously ensured their pharmacists and pharmacy technicians have access to SCR, as this was originally a requirement of the Pharmacy Quality Scheme.
Situations where consistent and reliable access to SCR may be outside the control of the contractor could include the SCR system being down at a national level and internet connection problems or power supply issues which the contractor has reported and their provider is seeking to fix. A failure to ensure a new pharmacist or pharmacy technician member of staff or a locum has a working NHS Smartcard which allows access to SCR would be a circumstance within the control of the contractor.
Pharmacy contractors with access to a more detailed record system such as their Local Health and Carer Record (LHCR) and access to SCR maintain access to SCR. SCR could be used as a backup in the event of an outage with the LHCR system.
Liability
The National Pharmacy Association has provided to NHS Digital the following statement:
“NPA indemnity Insurance will cover members’ access to the SCRs (and associated liabilities) where the pharmacist/pharmacy technician considers it necessary to do so (as well as any amendments the pharmacist/pharmacy technician decides to make to the SCR when this facility is enabled and available in the future) provided that this is done in line with available published guidelines, the pharmacy’s standard operating procedure (SOP) governing consent and access to SCR and use of the information therein.”
Numark Ltd has provided to NHS Digital the following statement:
“Numark Insurance recognises the potential for significant enhancements to patient care that access to SCRs represents. As such, our policy will provide cover to pharmacists and technicians utilising and operating within approved guidelines and continuing to act with due regard to patient safety, care and consent.”
The General Pharmaceutical Council released a statement regarding liability:
“Pharmacists’ access to patient medical records is a welcome and positive step towards enabling pharmacy professionals to deliver improved outcomes for patients. We believe that access to records will increase dialogue and communication and improve collaboration with other healthcare professionals. Whilst this is not a new area for some of the profession, for example those working in hospitals or those who work as prescribers, we recognise that this is a developing area for community pharmacy.
A pharmacy professional’s responsibility is to make the care of patients their first concern. Pharmacy professionals who can access patient medical records must ensure that they apply the principles and requirements of conduct, ethics and performance to any additional information that they can access as result of these changes. Our standards make clear a Pharmacy professional’s responsibility in relation to confidentiality and consent, as well as ‘getting all the information you require to assess a person’s needs in order to give the appropriate treatment and care.
Pharmacy owners are required to meet the GPhC’s Standards for Registered Pharmacies. Under the first principle in those standards, concerning governance, standard 1.7 requires information to be managed so as to protect the privacy, dignity and confidentiality of patients and the public who receive pharmacy services. Our inspectors would explore the pharmacy team’s use of the record as one evidence source when assessing the pharmacy’s performance against the standard.”
Use of other health records
Within some areas of England, pharmacy contractors may be accessing Local Health and Care Records (LHCRs). For example the Dorset Care Record can be accessed by pharmacy contractors.
These include additional information in comparison to SCR and there is an ambition for LHCRs to later enable ‘read’ and ‘write’ access to pharmacy teams.
Contractors may opt to access a LHCR record as an alternative to SCR access for relevant scenarios. However, even for contractors which opt to use LHCR as much as possible instead of SCR, SCR is a useful back-up e.g. in case the LHCR system experiences a technical outage. Consistent access to SCR is required as described above.
Read more about LHCRs at: cpe.org.uk/lhcrs
NHS Digital and Community Pharmacy England have received a number questions about SCR and have prepared these Q&As in response:
Preparing to use SCR
Q. How do I find about local training events in my area?
A. As these events finished in mid-February, a new process will be announced in the coming months for those who have not been to an event and plan to go live with SCR. Community Pharmacy England will issue news once the new process is confirmed.
Q. What do I need to do to get live, where is my pharmacy within the process?
A.There is a checklist of items to complete at cpe.org.uk/scrlist. Also read more on the NHS Digital implementation guidance document.
Q. As a relief pharmacist within a multiple organisation who is the person that should provide my face-to-face training briefing event and how should I get my Smartcard SCR-enabled?A.
A. Your pharmacy superintendent will be able to advise on how your organisation is going live with SCR and how you can get your Smartcard activated for SCR. Smartcards require adjustment to enable SCR – although this should be able to be done remotely.
Q. What is the process for locum staff with the 5F Smartcard wishing to gain SCR access onto that Smartcard? What if there is delay?
A. There will be a process for locum users to be able to access SCR. The locum Smartcard 5F may be used, frequently this may be provided where the staff member works at 5 or more pharmacies at short notice. In addition locum staff can then also add many regular premises to their Smartcard so that they can log-in using those rather than the generic F code.
If there is a delay with obtaining the required SCR codes onto locum Smartcards, for more than two weeks after the required paperwork has been submitted, then please refer to the Smartcard escalation route and/or you may contact your SCR Implementation Manager for further advice based on where you are located (contact information at end of this document).
Q. Where is the SCR Acceptable Use Agreement (AUA) for me to sign? What are the steps needed to sign this?
A. Here is the link to AUA form: https://nhs-digital.citizenspace.com/comms-iau/scr-user-agreement/ and see other criteria for going live listed at cpe.org.uk/scrlist.
Access to SCR
Q. I would like to check whether the pharmacy where I locum is live with SCR?
A. You may contact your SCR Implementation Manager for further advice based on where you are located (contact information at end of this document).
Q. Can SCR be accessed from any standalone computer using a Smartcard reader?
A. SCR can be accessed on a pharmacy PMR system that is on the N3 network e.g. pharmacy computer in the pharmacy. It cannot be accessed from home on a laptop. It can only be accessed on the N3 network with access via a Smartcard. If you have another PMR system terminal in another location in your pharmacy and if it is connected to N3 network and has a Smartcard reader, you can access SCR.
Q. Which technicians can access SCR?
A. Only Pharmacy technicians that are registered with General Pharmaceutical Council (GPhC) can access SCR. Initially, only the regulated roles by GPhC e.g. pharmacist and pharmacy technician can access SCR. The SCR team is exploring how other types of pharmacy team members could have access to SCR e.g. pre-reg, dispenser. All registered technicians that require access to SCR must complete the CPPE SCR eLearning module.
Using SCR and practising usage
Q. Could we have a test ‘Mr Nobody’ test patient account to access, to become familiar with SCR at our leisure, without a patient waiting?
A. You can use these test patient NHS numbers to practice SCR access and become familiar with the process: 999 040 2132, 999 025 2947, 999 025 2955, 999 024 3271.
Q. What is the website address that we need to use to access SCR? Will our chosen pharmacy system supplier have compatibility with SCR?
A. Link to access SCR website is here: https://portal.national.ncrs.nhs.uk/portal/dt
Your pharmacy system supplier needs to allow access to Internet Explorer on web browser for SCR access (see cpe.org.uk/wes)
Q. Is there a step-by-step guide on using SCR and finding the necessary information on the system?
A. Resources include:
- NHS Digital SCR usage guide
- Community Pharmacy England webpage ‘Using SCR’
Consent / auditing / emergency access
Q. If I have a query with a repeat prescription patient, given the patient will not be on-site, can I phone the patient to gain consent?
A. SCR can only be accessed if you have consent from the patient e.g. in person or over the phone. But for repeat patients you can have a one-off consent conversation which provides access consent for 12 months. You should record this permission in PMR patient notes field for the patient. For information on emergency access see the question immediately below.
Q. What is SCR emergency access?
A. Emergency access is SCR access without consent of the patient where the pharmacist/pharmacy technician has exhausted all options to obtain consent e.g. in person or by phone – it is access where the pharmacist/pharmacy technician makes a professional decision to access SCR in the best interests of the patient in the provision of care.
Q. What risk is there that I could be seen over-using SCR?
A. It is up to healthcare professional to decide how/when they access SCR in the provision of care to patients, when it is used in relation to their care. Some pharmacies use SCR frequently each day. The person auditing usage may check a proportion and that there is a patient, but should not need to check the clinical determination.
Creation and updating of SCR records
Q. How is the SCR created?
A. Summary Care Records are created and maintained by GP practices. The GP IT systems that they use, in accordance with GP IT Futures, have the capability to upload SCRs for all registered patients in a GP practice to the national NHS ‘Spine‘.
Records are then maintained automatically, whenever there is a relevant change to the patients practice record (and the user has logged on with their smartcard).
GP practices also have the capability to access and view SCRs for any non-registered patients including emergency and temporary patients.
As soon as a practice starts creating SCRs they are considered to be live with SCR. Any patient that is either seen at the practice, or whose information on their local record is updated, will have their SCR updated through the creation of a GP Summary Update.
Q. How is the SCR updated? Is there a requirement for GP practices to update the SCR?
From April 2014, GP practices were required to enable automated uploads of any changes to a patient’s summary information in the medical record, at least on a daily basis, to the Summary Care Record (SCR). Practices were required to implement this requirement as soon as possible after 1 April 2014 and should, by 30 September 2014, have published a statement of intent at the practice premises and on the website (where applicable) to achieve the requirement by 31 March 2015.
The requirement is on the basis of the current definition of the SCR i.e. the core SCR record contains medications, allergies and adverse reactions and is uploaded on the basis of implied patient consent. Additional information can only be uploaded with explicit patient consent and should be information required to support patient care in an emergency or urgent situation.
Shielded Patient List (SPL) and flag
Q. Is the Shieled Patient Flag still visible within SCR?
No.
The SPL was a record of vulnerable patients thought to be at high risk of complications from coronavirus (COVID-19).
An updated NHS SPL was generated weekly by NHS Digital, incorporating additional patient data provided by acute trusts, GP practices and other data sources. The list meant the SCR records could include a ‘Shielded Patient Flag’ (previously also called Vulnerability flag) where needed. This enabled community pharmacy teams using the SCRa application to see an alert when viewing the SCR of such a patient. The Shielded Patient Flag went live from April 2020. Following the government announcement in September 2021 regarding the end of national shielding in England, the SPL for England closed and changes to patient risk status stopped being applied. This meant: any changes to local patient risk status were no longer captured in the national SPL, or shared with other health and care system partners; and the high-risk flag is not an indicator to be relied upon to assess a patient’s current risk from COVID-19 by GPs or in practice management and reporting. Information contained in the SPL was last updated at the end of September 2021. As of November 2021, NHS Digital planned to undertake a managed closure of the SPL during late 2021 and early 2022 and planned to issue further communications later.
Following the end of shielding, NHS Digital has been instructed by Department of Health and Social Care and Joint Committee on Vaccination and Immunisation (JCVI) to change the high-risk flags in medical records, associated with previously clinically extremely vulnerable (CEV) patients, to a moderate or low-risk flag. This is part of a managed closure of the List.
As part of this, an engagement exercise took place with those who had used SPF to fully understand any continuing or additional use cases of the SPL. The aim of the engagement was to minimise the impact of closing the list on local services. NHS Digital engaged with a range of audiences including Community Pharmacy IT Group (CP ITG), hospital trusts, local authorities, mental health providers, and GP IT suppliers.
The “COVID-19 Risk Indicators” section, which was previously added to the “Key Demographic Information” page, and the associated alert within the Summary Care Record application was removed from all patient records during June 2022.
Resources include:
If you have queries on this webpage or you require more information please contact it@cpe.org.uk. To share and hear views about digital developments with like-minded pharmacy team members, join the CP Digital email group today.
Return to the Pharmacy IT hub; Electronic Health Records & SCR home or IT a-z index