Computable dose instructions standards
Published on: 26th January 2018 | Updated on: 7th April 2022
 The NHS Dictionary of Medicines and Devices (dm+d) provides a standard description and electronic identifier for all medicines but at present there is no standard structure to represent dosage instructions, for example, “Take two tablets three times a day.” Without this standardisation, this information can only be sent and stored electronically using ‘free text’/text strings.
The NHS Dictionary of Medicines and Devices (dm+d) provides a standard description and electronic identifier for all medicines but at present there is no standard structure to represent dosage instructions, for example, “Take two tablets three times a day.” Without this standardisation, this information can only be sent and stored electronically using ‘free text’/text strings.
Consideration has been given to developing standard ‘Computable Dose Instructions’ so that this information can be sent in a standard coded format, which will enable diverse clinical systems to manipulate the data transferred, for example calculate a dose or quantity. This will also improve patient safety by standardising the way that dosage instructions are communicated and reducing the potential for misinterpretation.
The International Journal of Pharmacy Practice, 23 (Suppl. S2 2015), pp. 23–105 evaluated a sample of prescription dose instructions and found that:
- 39.9% of prescriptions contained dosage instructions which were identified as requiring intervention;
- 25.2% items were identified as requiring to be edited in the pharmacy to improve quality and clarity;
- an extensive re-write was recommended for 14.7%; and
- of these the instruction ‘as directed’ was present in 3% items and 2% were prescribed with instructions containing Latin dose abbreviations.
The paper concluded that “there is an urgent patient safety need to establish a standardised format for written dosage instruction for inclusion on EPSR2 prescriptions”
Currently, the EPS messages use free text for dose information. The lack of an information standard for dose data is particularly an issue when drug information is transferred between primary and acute care service providers as their methods for describing dose and product are quite different.
The Professional Record Standards Body’s (PRSB) e-Medication Standards Requirement (2015) also explained that:
“Dose syntax needs to be standardised to enable dosage instructions to re-used when transferred between care settings. Until this is achieved, human intervention will be needed, i.e. the recipient will need to translate the instruction if it is not in the format used in their e-prescribing system.. Dose syntax is an important component of the medication record and work on it should be linked into the discharge summary.”
In summary, an effective dose syntax is expected to:
- improve patient safety by avoiding manual transcription errors in the care delivery process;
- support more intelligent patient outcomes analyses for drug prescriptions;
- assist managing work related to communicating dose data from prescription through to dispense; and
- be welcomed by the pharmacy profession.
Professional Record Standards Body has worked with NHS Digital, Community Pharmacy England, health and care workers and other stakeholders on its standards for medication dose and timings.
The PRSB website includes updated materials about the standard and related work within the ‘Digital medicines’ section of the website.
PRSB, Community Pharmacy England and CP ITG and others now want to see pharmacy, GP practice and other clinical system suppliers rollout the use of the standard – see section below.
Progress with supplier implementation of the PRSB standard is set out below.
Pharmacy systems
| Progress with integrating with the dose standard? |
|
| Analyst PMR (Positive Solutions (PSL)) | tbc |
| Colombus (Boots) | tbc |
| CoMPass (Lloydspharmacy) | tbc |
| Pharmacy Manager/Nexphase (Cegedim Rx) | tbc |
| ProScript Connect (EMIS Health) | tbc |
| RxWeb (Clanwilliam) | tbc |
| Titan (Invatechhealth) | tbc |
GP systems
| GP practice system suppliers | Progress with integrating with the dose standard? |
| SystmOne (TPP) | tbc |
| EMIS Web (EMIS Health) | tbc |
| Vision (InPS) | tbc |
| Evolution (Microtest) | tbc |
Community Pharmacy England and Community Pharmacy IT Group (CP ITG) long supported it being a key priority for systems to integrate with dose standards e.g. pharmacy systems and GP practice ones.
Information about related work prior to 2018 is set out below:
Standard Computable Dose Instructions were developed some time ago by the NHS Information Authority and Connecting For Health (now NHS Digital) in conjunction with the international health standards organisation, HL7. This model was considered too complex for routine implementation, and a simplified model was further developed. The work has received some global interest because of its value across national borders.
In 2015, PRSB commented within its e-Discharge Summary Implementation Guidance that the future standard Computable Dose Instructions involved an:
“intended direction of travel is to move towards a future:
(a) where all health care prescribing systems express drug names using dm+d coding both for product based and for dose based prescribing; and
(b) where all health care prescribing systems can also generate a parsable dose directions string that will incorporate all of the remaining information beyond the drug name that is essential to express an unambiguous prescription.
Through a combination of using dm+d and also parsing of these structured dose strings it should then be possible to convert a dose based prescription to a semantically equivalent product based prescription and vice versa. Depending on the structured dose syntax solution eventually adopted it is anticipated that upwards from 80% of all prescriptions could be automatically converted between dose based and product based expressions of prescriptions. Components are already included in the Medications and medical devices information model to support structured dose syntax and its processing.”
NHS Scotland had commissioned some work for the project to build on previous efforts. The Scottish Clinical Information Management in Practice (SCIMP) published their 2015 NHS Computable Dose Instructions project recommendations. SCIMP recommended next steps to include:
- further work on the drafted dose syntax;
- preparation of implementation guidance for prescribing system suppliers, for their consideration and feedback; and
- NHS England open source project to consider involvement.
The Data Coordination Board’s (DCB) predecessor, SCCI has also considered next steps that relate to the Scottish and English project work:
- it needs to incorporate clinical as well as academic input;
- the focus should initially be on routine prescribing as this is where the most volume is;
- it may require and benefit from a consortium based approach, involving suppliers and the user community; and
- the works relationship to other standards such as SNOMED CT and GS1 will need to be defined.
A PRSB 2015 e-Medication Standards Requirement included some recommendations about the Computable Dose Instructions project:
- “..On-going awareness raising, engagement and education [could take place] focused on encouraging take-up of structured coded discharge message including dose syntax
- “Establish a work programme to address gaps/issues (starting with dose syntax, using the work already underway).”
- “..difficult to translate electronically at transfers of care. Development of a dose syntax standard across care settings should address these issues and has already progressed well in Scotland..”
- “..The dose syntax work needs to be closely linked into the development and implementation of discharge summary messages as it will be key to enabling medication information in the summary to be incorporated into the GP record.”
- ..In progressing the work, HSCIC [now NHS Digital] should take account of the work already completed (medication model) or underway (dose syntax and drug allergies). It will be essential to take a co-ordinated approach across the four nations as all have plans to implement hospital e-prescribing and medication administration systems over the next few years and to implement communication of medications between primary and secondary care. It will be cost efficient to share the standards work. As the same primary and secondary care suppliers work across the four nations, common standards should also be cost effective.
- “Work, which Leo Fogarty [had been] leading, on dose syntax parser for primary care and at least partially for secondary care. This is currently being validated with suppliers.”
- “Leo Fogarty is leading work on dose syntax. There is also uncompleted [NHS Digital] work on dose syntax. These take different approaches, so a first step would be to decide on the agreed 4 country approach and then take forward in consultation with general practice and hospital users and system suppliers.”
- “[There is] impact on the dose amount and timing instructions which makes these difficult to translate electronically at transfers of care. Development of a dose syntax standard across care settings should address these issues.”
SCIMP met in April 2017 in Falkirk, Scotland. They published a detailed report of the SCIMP meeting and also a short statement called ‘The Falkirk Declaration’. The agreement stated 11 principles and further steps:
- There is a clinical requirement to improve the safety and effectiveness of the management of medications at transitions of care
- The NHS in the UK are addressing this through a number of linked professional and governmental organisations, e.g. NSS SCIMP, PRSB, UKTC, interOPEN, Care Connect
- These have now agreed clinical medication models and data exchange standards for sharing medication data
- These agreed models and standards should thus be used by projects and programmes using electronic medication records, including linked systems
HL7 FHIR profiles are being adopted by vendors to the NHS in the UK, expressed from international FHIR medication resources, and so becoming the de facto interoperability standard - The dm+d is also now the de facto standard drug dictionary for the NHS in UK
Computable Dose Instructions have now been designed using interoperable resources, and shown in pilots to be components fit to contribute to the first purpose above - This set of models and standards must be a non-proprietary resource, openly distributed and available to contribution from all stakeholders
NHS bodies must support this by procuring only systems which conform to these standards - This infrastructure upgrade policy requires evaluation on wider bases than the short-term financial, to include clinical time saved and harms reduced
- The clinical community require that these technical models are developed in response to clinical requirements, and to be assured of their clinical safety
- The resources to gather requirements from clinical teams must:
– produce medication systems that are safe, effective and person-centred in their application
– be supported, co-ordinated and collaborative - There shall be implementation of these recommendations by NHS bodies in each of the NHS in UK
- NHS Scotland must formally engage with this UK work to ensure local operational and clinical requirements are modelled and that it has the skills and knowledge to use the resources
Back in 2017 NHS England have commissioned interOPEN and PRSB to collect together Fast Healthcare Interoperability Resources (FHIR) implementations of Medication profiles used in GP Connect to automate messaging across Transfers of Care, as medication reconciliation work is a high burden on clinicians. As of February 2018, Computable Dose Syntax was not yet formally started as a project, but the related medication messaging is being designed to be forwards-compatible with a future Computable Dose Syntax.
The work done then evolved into a full set of models that was seen at the openEHR CKM tool at https://openehr.org/ckm/#showProject_1013.30.27. These models went beyond the scope of the original community prescribing ‘dose syntax’ into full inpatient and outpatient prescribing models but are now being used inside real hospital and community prescribing systems in various parts of the world but based on an approach established by previous NHS Scotland work established in ‘Dundee’.
Structured dose/timing was left out of scope of the first FHIR profile collections. Supplier commitments were needed for work to progress, and also the FHIR versions of dosage/timing require additional testing compared to the openEHR (Electronic Health Record) models referred to earlier. NHS Digital and PRSB further developed standards for England for prescribing and dispensing suppliers to adopt and use for their users – read more within the other sections of this webpage.
Further info
If you have queries on this webpage or you require more information please contact it@cpe.org.uk. To share and hear views about digital developments with like-minded pharmacy team members, join the CP Digital email group today.
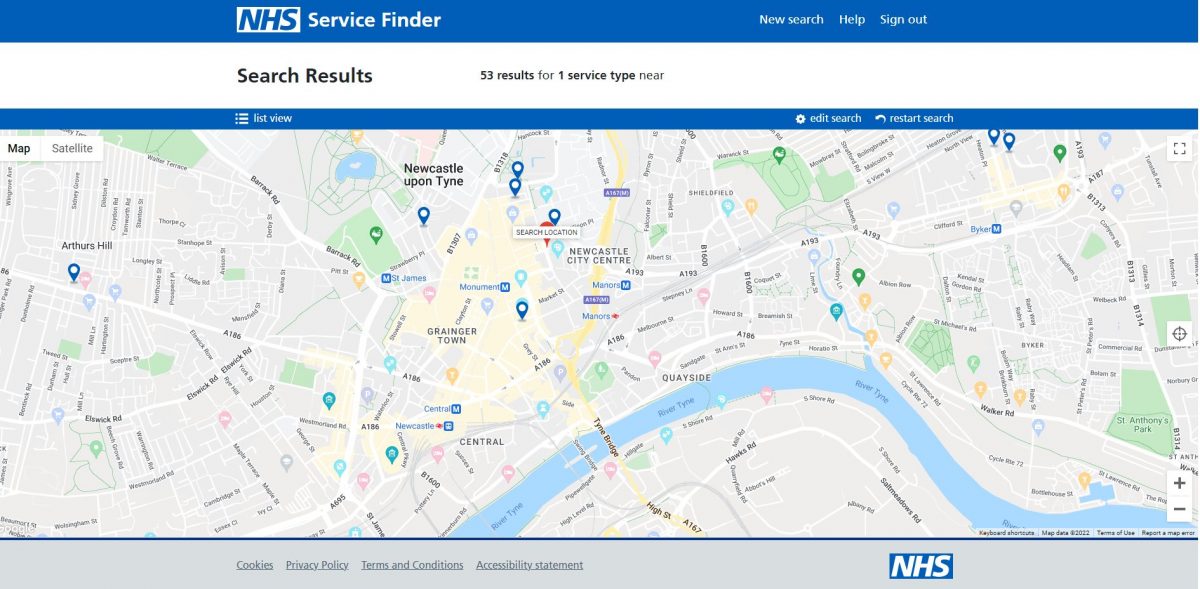
Return to the IT section: Standards and Interoperability