Community Pharmacy IT Group (CP ITG) workstream updates
Published on: 28th June 2021 | Updated on: 19th October 2023
Read more about CP ITG and its work at: the Community Pharmacy IT Group (CP ITG) webpage.
This ‘CP ITG workstream update‘ webpage sets out information following CP ITG meetings based on the the latest pharmacy IT bulletin.
The latest bulletin can also be downloaded in pdf format: CP ITG Summer 2023 IT bulletin update (pdf)
CP ITG has five workstream areas:
- Interoperability and security: Ensuring information about people’s health and care can be safely and securely accessed, wherever it is needed. (WS1a-1d)
- Reducing burden: Use of digital to reduce the burden on pharmacy teams, so they can focus on patients, and appropriate infrastructure for the task. (WS2a)
- Good use of digital: Support the use of digital within pharmacy to improve health and care productivity, improve patient safety outcomes and improve cooperation between pharmacy teams and the health and care system. (WS3a-3c)
- Patient and pharmacy tools: Support enabling patients to be able to choose digital tools to access medicines information and pharmacy services directly, so they can receive the best outcomes, recognising the need to also remain inclusive for all patients. (WS4a)
- Set out roadmap priorities: Development and promotion of a wider community pharmacy digital roadmap / vision. (WS5a)
See downloadable PDF version of the full: CP ITG workstreams.
These sections below set out updates related to these workstreams based on the most recent pharmacy IT bulletin.
PSNC becomes Community Pharmacy England
Community Pharmacy England is the new name for the representative body for all community pharmacies in England – from 30th May 2023. Community Pharmacy England will continue to work closely with everyone in the community pharmacy sector. Its goals are to develop the NHS community pharmacy service, to enable community pharmacies to offer a range of services that meet the needs of their local communities and provide value and good health outcomes for the NHS and the public. Its committee is made up of representatives of pharmacy owners in England from all parts of the community pharmacy sector. The name change reflects the organisation’s current and future work. Changes have been applied to the website: cpe.org.uk (and webpage redirects are in place) and its Digital and Technology section. The email contact points for CP ITG secretariat correspondence have been updated to it@cpe.org.uk and Daniel.Ah-Thion@cpe.org.uk (email redirects are in place if the older email addresses are used).
Overview of pharmacy IT priorities overview and brief update on the IT elements proposed within the Primary Care Recovery Plan
NHS England, DHSC and the CP ITG have previously flagged the pharmacy IT priorities: PRSB Community Pharmacy Data Standard / Community Pharmacy Contractual Framework (CPCF) IT; records access; payment and data APIs; Booking and Referral Standards (BaRS); and EPS next generation. The CP ITG has continued to support these projects and Community Pharmacy England is also working with the NHS on the next steps to progress these areas. These priorities align with the CP ITG’s vision and the ‘key to the future of pharmacy IT’ infographic (which incorporates requested updates from CP ITG and pharmacy reps. The Primary Care Recovery Plan sets out digital enablers in line with these (see the IT policy: Delivery plan for recovering access to primary care section).
Payment and data Manage Your Service (MYS) APIs for CPCF services
NHS England and Community Pharmacy England want suppliers to be given information about the service, including the IT implications and dataset requirements. The MYS API priorities were previously listed as: Pharmacy Contraception Service, Discharge Medicine Service (DMS), Blood Pressure Checking Service, New Medicine Service (NMS) and the Smoking Cessation Service. CP ITG pharmacy representatives previously reported that data entry for services such as DMS is taking a large amount of pharmacy teams. During April 2023 NHSBSA released an expression of interest for the DMS API to explore interest with the market providing this integration service. NHS England and NHSBSA had been committed to prioritising API programmes progress within 2023/24 delivery plans.
Update on Professional Record Standards Body (PRSB)’s Community Pharmacy Data Standard (CPDS)
PRSB’s Community Pharmacy Data Standard (CPDS) remains critical for enabling:
- the community pharmacy sector being able to record and transfer data in a consistent and structured way;
- suppliers to use a blueprint; and
- other parts of healthcare and the NHS from receiving information in a structured format.
NHS England commissioned PRSB to uplift CPDS. The uplift was to reflect changes to the Community Pharmacy Contractual Framework in England and for purposes of futureproofing. PRSB arranged two webinars: a supplier meeting (2nd February 2023), and a general webinar (7th February 2023). CP ITG participants were encouraged to attend these. CP ITG have also been provided with email updates about the project during the months after those. The uplift plans were set out within this slide-set. An Information Standards Notices (ISN) application was approved by Data Alliance Partnership Board (DAPB) subject to approval of the clinical safety case by the NHS England Transformation Directorate’s Clinical Safety Group (CSG) which is likely within June 2023. The ISN specifies implementation by suppliers during 2024 calendar year and compliance by end of March 2025. Implementation support for suppliers from PRSB is awaiting business case approval in NHS England. Queries relating the standard can be directed to support@theprsb.org or the PRSB Standard support query webform.
Supporting NHSmail
- Community Pharmacy England published a factsheet for community pharmacy teams explaining how to access the shared NHSmail inbox within the Outlook mobile app.
- The Virtual Visits tool provides pharmacy members with an appointments system so that they can notify patients and better manage appointments. Pharmacy teams can also use the Virtual Visits tool to conduct face-to-face or virtual patient consultations (audio or video).
- The Virtual Visits tool works in conjunction with NHSmail Microsoft Teams and the Microsoft Booking platform. To participate in the pilot, you must have an active personal NHSmail account, access to a shared NHSmail inbox, MS Teams installed on a computer or tablet and a computer or device with a webcam. Pharmacy members can now:
- register interest with taking part in the Virtual Visits pilot via this webform;
- view the one-page factsheet about How Virtual Visits works; and
- consider the guidance checklist.
NHSmail multi-factor authentication (MFA)
- MFA is already a requirement for Welsh NHSmail. CP ITG previously fed back to the NHSmail team that clear communications and proper testing should occur prior to a full roll-out of MFA across pharmacy NHSmail users. Community Pharmacy England and the NHSmail team have worked on guidance to support the testing of MFA.
- MFA will be an important development for NHSmail. It helps data to be kept within a more protected environment. It helps protect the reputation of the NHS, and the individuals and organisations that use NHSmail. It also provides increased protection against cyber-attacks. The NHSmail plan is to make MFA mandatory for all NHSmail users. The NHSmail team expect most organisations to have fully implemented MFA within January to March 2024. Mandatory rollout of MFA for the PODS NHSmail users (pharmacy, optometry, dentistry and social care, DACS, Independent Midwives, GP Locums) is currently scheduled for January 2024.
- Community Pharmacy England working with the NHSmail team has a prepared new one-page factsheet for those pharmacy NHSmail users testing MFA (or adding/removing MFA).
- Next steps:
- Pharmacy representatives can feed back about the preferred MFA options.
- Pharmacy representatives are also encouraged to urgently put themselves forward to test out MFA by using the guidance factsheet to switch MFA on. Pharmacy representatives are encouraged to submit comments to it@cpe.org.uk about piloting experiences and comments on the new guidance for MFA pharmacy testers.
Recommended minimum transfer dataset for pharmacies switching from one patient medication record (PMR) system to another
- Community Pharmacy England previously supported developing a recommended minimum dataset for cases where a pharmacy member has switched from one PMR system to another. For the sake of continuity of patient care, it is critical for some patient information to be transferred from the old to the new system.
- Community Pharmacy England has worked further with a CP ITG sub-group on the minimum agreed minimum dataset and associated transfer specification document during March-May 2023. This has resulted in the documents being iterated to 0.99 versions:
- Version 1.0 is expected to be promoted from late June 2023.
Standards
NHS England are conducting a dm+d survey about further changes to virtual medicinal product (VMP) drug forms. This survey was originally going to close in April 2023 but the close data has been extended. CP ITG suppliers in particular were (and are) encouraged to take part.
CP ITG inputs about pharmacy IT supplier development
Community Pharmacy IT Group were asked to feed into “Items for pharmacy IT supplier development” infographic. The feedback from pharmacy representatives and supplier representatives is set out on the next page. Further feedback is welcome from all pharmacy team members. Please contact it@cpe.org.uk with comments by the end of June 2023 so that your comments can be incorporated into the next iteration of the infographic.
Pharmacy IT development: technical and commercial approaches via the NHS Digital Care Services Catalogue
NHS England previously fed back it continued to explore commercial requirements and opportunities that will support both the needs of the sector and system suppliers now and in the future to support and develop an open supplier market. Currently there is not a comprehensive framework for NHS England to incentivise community pharmacy IT system suppliers to make technical developments that would align with the objectives within the NHS Community Pharmacy Contractual Framework (CPCF). NHS England are seeking to put a process and framework in place to enable this across pharmacy and other sectors. NHS England’s Transformation Directorate plans to support community pharmacy suppliers moving onto the Digital Care Service Catalogue (which is also used by GP IT Futures framework). NHS England’s Transformation Directorate hosted a kick-off call with suppliers and some Community Pharmacy IT Group representatives on 26th April 2023. A meeting recording is available for relevant participant organisations.
- A Prior Information Notice was issued to the market (including CPCS suppliers) on 1st June 2023 including:
- Digital Pathways Framework;
- Legacy Foundation Solutions Framework (periodic refresh of GP IT Futures Framework);
- Primary Care Support Services (period refresh of GPIT Futures with greater scope definition);
- Detained Estate (covers the estate in England and Wales, single clinical system);
- Research Development & Engagement (opt in Framework facilitating direct agreements between NHS England and parties); and
- Engagement with Community Pharmacy regarding CPCF Digital Service Standards & Roadmap.
- Supplier Expression of Interest (EOI) Forms were available with deadline midday 16th June. Further NHS England discussions with the community pharmacy supplier community are anticipated over June 2023 fortnight. NHS England’s Transformation Directorate are planning to publish supportive documentation for suppliers.
Pharmacy Contraception Service IT
NHS England announced that Pharmacy Contraception Service (PCS) commenced as an optional Advanced Service for community pharmacies from 24th April 2023. On 9th May 2023, the Government and NHS promised investment in community pharmacies over the next two years, part of which could support the expansion of the NHS Pharmacy Contraception – and NHS England and Community Pharmacy England are to consider the details of such an expansion.
It has been a soft launch with minimal communication to the sector and to respect the current sensitivities around workforce and financial pressures and the feedback from Community Pharmacy England on behalf of its pharmacy members.
Most engagement has been done through regional teams that are supporting pharmacy teams that opted to engage during this earlier stage of rollout. The key requirement of the specification is for the pharmacy members to use an approved IT solution (current options are the Cegedim and PharmOutcomes which are being provided free of charge until April 2024 while other IT supplier commercial models may vary). As of June 2023, 1,600 pharmacy members had registered to provide the service. The team mentioned that they have had positive feedbacks from Cegedim and PharmOutcomes, on the end-to-end API having been made available early, there were no reported IT issues and pharmacy feedback to NHS England is that they are finding the IT easy-to-use, particularly when they self-populate.
The post event message for GPs which can be automatically populated is saving time compared to what pharmacy teams had to do during the pilot.
Services IT
- NHS England announced that the way some Community Pharmacist Consultation Service GP referrals are sent by the EMIS PharmRefer product is changing.
- Pharmacy representatives that use an Point of Care vaccination system, who would like to share how these can develop etc, please email it@cpe.org.uk and you can be put forward for potential participation within an NHS user researcher project.
Urgent treatment centres and emergency departments can now refer patients to community pharmacists
NHS England update: “Urgent treatment centres and emergency departments can now start to refer patients for a consultation with a community pharmacist for a minor illness symptom or for an urgent supply of a regular medicine, using an IT solution which meets the minimum digital requirements of the service (as specified within the NHS Community Pharmacist Consultation Service Technical Toolkit). A toolkit of supporting information, including an updated CPCS specification, can assist regional and ICB teams with mobilisation plans. From 1st June 2023 in a change from the previous service specification, claims for payment should be submitted within one month of, and no later than three months from, the claim period for the chargeable activity provided.”
Electronic Prescription Service (EPS)
- Pharmacy teams are encouraged to complete the EPS Paperless, Outcomes and Trackability survey (5- 7 mins). The results are feed into a study by Kinston University and will also be shared to the NHS England EPS team. Community Pharmacy England has promoted this survey.
- The NHS EPS team will be seeking more feedback from stakeholders and capturing feedback through one-to-one sessions during summer 2023 and potentially beyond. This engagement will capture further views regarding EPS trackability improvements. EPS user research team sessions will be run in a similar fashion as was done last year i.e. a remote interview and review of any prototyped screens. We’d encourage you to register interest with participating by using this signup form if you’ve not previously listed yourself: https://feedback.digital.nhs.uk/jfe/form/SV_eu4jQRNbJooQxoO.
- Business Leader reported that Titan PMR becomes first NHS accredited software for dispensing doctors.
Real Time Exemption Checking (RTEC)
- The NHSBSA continues to lead the RTEC project. The NHSBSA, DWP and the RTEC steering group plan has supported the expansion of the DWP RTEC functionality to additional pharmacy members. The group may suggest items for the RTEC development roadmap by emailing it@cpe.org.uk.
Independent prescribing IT
- The General Pharmaceutical Council (GPhC) previously consulted and reported on changes to the requirements for entry to independent prescribing courses, and the Pharmaceutical Journal reported that independent prescribing piloting was to begin across England from 2023. NHS England previously reported into the CP ITG about the plans for the pathfinder programme.
- CP ITG Chair, Matt Armstrong is taking part with NHS England’s independent prescribing pathfinders’ operational group on behalf of the CP ITG. This group will play a key role with supporting the programme and the evaluation that will inform longer term strategy for introducing independent prescribing into community pharmacy clinical services and providing input to the requirements for EPS system to support pathfinders.
- NHS England pharmacy team are awaiting the outcome of Moderation and hoping to inform Integrated Care Boards of their successful Expressions of Interest soon.
- Ppharmacy teams are encouraged to complete the Independent Prescribing Programme & IT survey (5-7 mins).
Digital first
The government has previously set targets for increasing the digital options for patients using the NHS e.g. ability to book appointments online and to order repeat prescriptions online. NHS App is one app which provides such functionality but other apps and websites aligning to relevant NHS IT standards are also increasing digital patient interactions. NHS App updates are outlined within the NHS App section below. Further workshops are to be planned regarding apps and NHS App developments. CP ITG will be invited to those. If you are use an app or provide an app to pharmacies, and would wish to take part please contact it@psnc.org.uk within June 2023 with ‘Apps event’ within the email subject title.
Patient experiences of systems and equality considerations
Case study in West Yorkshire: West Yorkshire is a multi-cultural region of England, where a diverse number of languages are spoken by people as a first language. A percentage of this demographic have a limited proficiency in English, a language that all prescriptions and pharmacy labels are printed in. NHS West Yorkshire Integrated Care System (WY ICS) & North of England Commissioning Support Unit (CSU) are supporting a pilot in which community pharmacy teams and hospital pharmacy teams can use IT to provide translated medicine dose instructions. At this time only one supplier met the criteria for initial participation within the pilot: Written Medicine. The Pharmacy Terms of Service do not set out requirements for translation activity however pharmacy teams that participate within the pilot receive the software and receive funding towards their work and costs involved. Community Pharmacy West Yorkshire are feeding into the pilot. The pilot findings are to be evaluated by a local university. Lots of patients are not taking their medicines correctly and a portion of this is likely to be due to language challenges. Pictograms/illustrations and audio files are also being added, broadening the application to meet all accessible information and reasonable adjustment needs (although this is not yet part of the pilot). The pilot areas are West Yorkshire and Harrogate – an area in which the solution will be helpful for a larger segment of patients. The pilot prioritises hospitals and community pharmacies and it will be launched from July 2023, and further volunteers will be sought. The pilot team is consulting a stakeholder group which includes Community Pharmacy West Yorkshire. The pilot may run for six months from September, depending on the uptake and other factors.
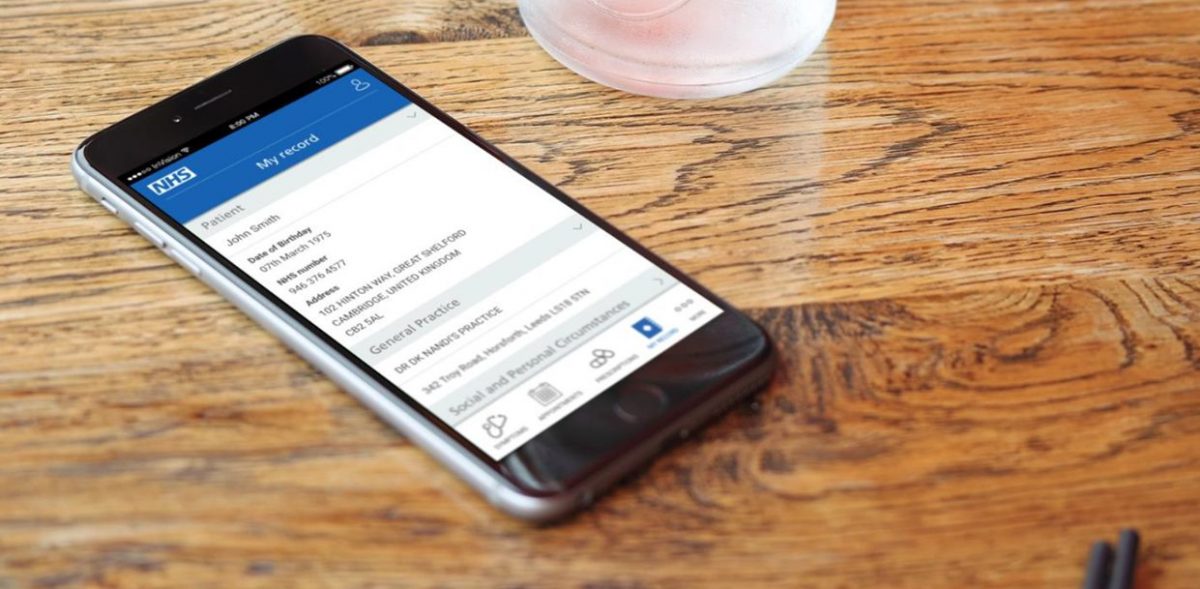
NHS App objectives
The NHS App team say their overall objectives 2023/24 are the below.
- Maximise value from the NHS App by increasing self service and self care to aim to reduce demand on the front line.
- Continue developing appointments, record access and prescriptions capabilities to keep up with policy and emerging user needs.
- Continue to develop the design and navigation of services to address user needs.
- Continue to enhance the messaging capability to improve the experience for senders and recipients.
- Ensure the NHS App team understand enough about all users’ behaviours and the full capability of the channel to help them to complete usable end to end journeys.
- Extend the integrated services available in the NHS App to support localisation and better meet users’ healthcare needs.
- Extend the underlying capabilities of the NHS App platform with a view to providing the platform capabilities for our future ambitions.
NHS App recent and future developments
The NHS App team are continuing to develop existing and future features. Selected developments are listed below. The full roadmap list is at: https://digital.nhs.uk/services/nhs-app/future-developments.
Recently completed:
- Integrated the National Booking Service so that people can book their Spring Covid vaccine booster using the app.
- Self-asserted blood pressure test results discovery, to understand what is needed to build a service that works for patients and practices.
Working on now:
- Digital Prescription Token discovery and scoping an online prescription ordering service for users without a nominated pharmacy.
- Improve the way that primary care data is sent to the app, to enable a richer, more user-centred experience. This work is often referred to as GP patient-facing APIs.
- Improve test results to allow patients to easily access and understand test results.
- Digitally requesting proxy access for adult to adults with capacity (private beta).
- Allow people to easily find and register with a GP within the app.
- Extend hospital appointment supplier integrations to give more patients access to improved secondary care appointment information.
- Simplify NHS App integrations with national services and other senders.
Working on next:
- Book and manage flu vaccinations via the app.
- Medicines A-Z from NHS App to give people easier access to information about their medications.
- Prescription order updates to users with repeat prescriptions.
- Improve hospital appointment supplier integrations to give more patients access to improved more secondary care appointment features.
- Enable people to update their postal address through the NHS App.
- Notifications relating to GP registration.
- Offering users communications about their covid vaccine appointment confirmations and reminders.
Other NHS account and NHS App updates
- Digital Health published an article on the NHS App being a critical tool in tackling the elective care backlog.
- Dan Collins, senior product manager for the NHS App, explained why the NHS App team want to open up the app to more suppliers offering online consultation services and welcomes the latest service to integrate.
- Rupesh Thakkar, implementation lead at NHS England, described how the repeat prescriptions feature on the NHS App impacted primary care services in his area.
- NHS England reported that the number of repeat prescriptions ordered via NHS App was up by compared with last year, although the majority of orders made digitally are made using other tools. The group’s pharmacy representatives previously commented that NHS App does yet notify the nominated pharmacy of orders preventing the pharmacy from having an ability to check whether the items ordered have been inadvertently missed from patients’ prescriptions.
- Digital Health reported on Newcastle Hospitals’ patient engagement platform integration with NHS App.
- The i reported that NHS App could allow patients to shop around hospitals for shortest waiting time.
Patient tools
- Community Pharmacy England reported on pharmacy use of patient apps.
- Boots Pharmacy described their approach for expansion of patient digital tools.
- NHS Digital explored using content types to transform the NHS website.
- NHS Digital announced that online GP registrations reached 240,000 as the new digital NHS service grows.
- Open Access Government reported on adopting a digital-first public sector service approach.
- The NHS Covid-19 app is to be discontinued on 27 April 2023 following a steady decline in the number of active users.
- Digital Health strategist Lia Ali discussed how bringing user-centricity into health innovation improves patient outcomes.
- BBC reported on the tech helping women manage the menopause.
- Medical Futurist reported on the landscape of skin-checking apps.
- The HearO smartphone app is in clinical trials to assess how it can predict heart failure deterioration using AI technology.
- Eight new NHS online therapy courses and apps were conditionally recommended by NICE to help treat depression.
- Imperial College London reported that a genetic test already used routinely in the NHS can guide the use of chemotherapy in people with bowel cancer, new research has shown.
- NICE backed digital therapies for depression within draft guidance.
- Northumbria University reported that Wearable device provided support for Parkinson’s patients.
- Organisation for the Review of Care and Health Apps (ORCHA) chief executive officer explained why digital health is essential to relieve pressure on urgent care.
- An evaluation was conducted of the myDiabetes tool, and findings drawn about whether such apps can improve education and ongoing self-management of healthcare. The summary findings of this study were that “there is potential for increasing diabetes education rates by offering patients a digital option in combination with traditional service delivery which should be substantiated through future research.”
Digital inclusion
- King’s Fund published: Ensuring digitally enabled health care is equitable and effective for all.
- The Department for Work and Pensions plans to make its digital services more accessible and improve data-sharing with the NHS as part of a range of reforms intended to improve disabled people’s experience of the benefits systems.
- Kingston University student helped launch UK’s first tech-led LGBTQ+ sexual health service.
Direct Care APIs and GP Connect Update/Access Record
GP Connect enables GPs and other authorised health care organisations to link in with GP system information, allowing those authorised to use additional access/update record functionalities. NHS England’s Transformation Directorate have updated the GP Connect further since the last workstream update.
The Direct Care APIs programme creates and manages multiple NHS IT products including the GP Connect products. The GP Connect products allow information to flow across health and care systems and geographical boundaries in a structured way in support of direct patient care. The vision of the Direct Care APIs programme is to provide a single mechanism to share information across health and care systems and across boundaries in support of direct patient care.
These are a mixture of GP Connect products:
- Access Record HTML: A read only view of the patient’s record held by the GP practice, including free text and coded entries but excluding documents and attachments.
- Access Record Structured: The patient’s full record held by the GP practice, in structured coded format which can be ingested and saved into the consumer record.
- Send Document: Send a PDF document from one care setting back to the registered GP Practice.
- Update Record: Send structured coded information back to the registered GP Practice to allow auto-ingestion of that information.
- Appointment Management: Book, amend and cancel appointments in a primary care setting.
- Patient Facing Services: supporting replacement of legacy technology to provide structured data into the PFS to drive ‘Mobile First’ citizen behaviour.
‘Access Record Structured’ and community pharmacy: In order to improve community pharmacy access to information, the development of Access Record will allow pharmacy staff to view patient information in their local systems. All GP system suppliers are either ready to proceed with first-of-type piloting or are currently in the ‘assurance stage’ (which is progressing well). NHS England would like to work with community pharmacy suppliers to ingest a tailored dataset from the GP to support the patient consultations of pharmacies.
‘Update Record’ and community pharmacy: To improve the flow of data from community pharmacy to GP Update Record will allow information relating to Medications dispensed, Observations taken and a summary of the encounter to be sent back to the registered GP and will be auto-ingested. The next time the patient record is viewed, the information from community pharmacy will be available as part of the ongoing patient GP record. Observations will also be made available via PFS solutions alongside observations taken at the GP Practice to support presentation of holistic patient observations. Technical specification is currently being reviewed by GP suppliers and will be shared with community pharmacy after this session.
Electronic health records usage within community pharmacy
- Community Pharmacy England reported on the Summary Care Record application portal being replaced by National Care Records Service.
- Shared Care Records (ShCR) are patients’ electronic health records. ShCRs include information from multiple care settings, e.g. GP practice and secondary care. Most English patients live within an area with a records project ongoing. Shared care records are emerging across the country and the IT has been maturing, with the aim being that over time more health and care professionals can access these records. LPCs and/or local pharmacy members can continue to take steps to gain pharmacy access and should use the guidance set out in the ‘Engagement’ section of Community Pharmacy England’s community pharmacy and ShCRs webpage.
- Community Pharmacy England has been encouraging pharmacy IT support to ensure that ShCR, NCRS and records links are authorised for use via communications with the CP ITG whitelisting mailing list.
- Community Pharmacy England continues to work with NHS England’s Transformation Directorate and other relevant stakeholders on the actions set out within the Shared Care Record (ShCR/LHCR) NHS Transformation Directorate and pharmacy outputs and actions LPCs, ShCR project teams and other parties supporting ShCR pharmacy deployment are encouraged to contact it@cpe.org.uk with any technical ShCR information so that supplier and IT support helpdesks can authorize multiple ShCR domains simultaneously.
Records: national
- Oracle Cerner’s vice president opined that the NHS should not treat the implementation of electronic patient records as IT projects and instead view them as a “transformation process improvement”.
- Digital Health published a special report on Usability and why secondary care electronic patient records systems (EPRs) can and should do more.
- HSJ reported that although electronic patient records are regarded as an essential to delivering better care, there is evidence that records systems without optimal usability may contribute towards clinician burnout.
- The GP Connect team conducted user research on the GP Connect Structured FHIR API solution, and CP ITG suppliers were encouraged to consider participating.
Records: local
- The Greater Manchester Care Record (GMCR) ShCR project team hosted a community pharmacy IT supplier kick-off meeting on 19th April 2023 and many of you will have attended. It set out potential integration work and the advantages for supplier s considering this – including funding contributing towards development. This webinar had explained:
- their records project and the footprint of nearly 700 pharmacies;
- direct award incentive funding offer to support pharmacy IT supplier development;
- ability for suppliers to develop Single-Sign-On and One-Click; and
- learning for future ShCR and NHS records interoperability work.
- The GMCR team were made aware that CP ITG reps including suppliers reps had fed back that improvements were needed to be made to underlying coding and protocols including NHS IT standards (so that fewer different integrations would be required for suppliers to plug into multiple NHS records systems).
- Saint Catherine’s hospice became the first to use the Yorkshire and Humber Shared Care Record.
- Mid and South Essex Integrated Care System commissioned the Patients Know Best platform for its patients, to support access to personal health care records.
- NHS Western Isles Health Board expanded its use of Cambric Systems’ Morse Electronic Patient Records app, which aimed to enable more joined up patient care within Scotland.
- Patients Know Best supplied more NHS trusts with personal health record solutions.
Genomics
- Source BioScience has opened a new Genomics and Precision Medicine Centre in Cambridge.
- CNN reported that 100,000 new-born babies will have their genomes sequenced in the UK -potentially with implications that may develop how child medicines are prescribed and dispensed in the future.
- BMJ published an article on genomics and patient expectations surrounding genetic risk factors.
Other records updates
- SCR AI changes continued beyond COVID-19 legislation which expired during 2022. Community Pharmacy England and the Community Pharmacy IT Group have campaigned for pharmacy teams’ access to SCR AI to be extended beyond the pandemic by sharing case study information. If you have any examples of how SCR with AI has enhanced patient care, in comparison to normal SCR access, please contact it@cpe.org.uk, as such examples could be used to support the case for permanent access to SCR with AI and other health records for pharmacy.
Standards and interoperability
- At a previous meeting, the group agreed to support the capability for anonymised data to be accessible, so that pharmacy teams’ interventions can start to be auditable, and the value of community pharmacy can be better demonstrated. If PMR systems were to be adapted to allow such data sharing, it would require the development of a roadmap and a standard approach to data provision, which may benefit from use of SNOMED CT clinical terms. If you would like to help with this work, please contact it@cpe.org.uk.
Data Security and Protection Toolkit (DSPTK)
- Community Pharmacy England updated its Data security and information governance hub and published new guidance documents for the 2022/23 Toolkit submission. Additionally, Community Pharmacy England and the NHS DSPTK team jointly presented a webinar on the topic, which around five hundred people registered to attend. The new DSPTK webinar was subsequently made available on demand. Community Pharmacy England and the NHS DSPTK team are working on the arrangements for the community pharmacy 2023/24 toolkit publication ahead of the next June 2024 deadline. If you would like to feed into the development of the 2023/24 toolkit, please email it@cpe.org.uk.
NHS IT services & older browsers
- Previous bulletins have provided updates regarding NHS IT becoming non-compatible with older versions of Internet Explorer (e.g. 7, 8, 9 or 10). NHS England’s Transformation Directorate security team have said that using unsupported browsers and systems makes organisations vulnerable to cyber security threats and performance may also be impacted. The Transformation Directorate have been communicating that some NHS IT services will no longer be compatible with Internet Explorer version 7, 8, 9 or 10 from 22nd June 2023. This may include NHS Spine application, Patient Demographic Services (PDS), MeshUI, Electronic Prescription Service Prescription Tracker, Spine alerts and Summary Care Record application (SCRa). NHS Credential Management and NHS Identity Agent software is also recommended for Smartcard authentication. Pharmacy IT support and Patient Medical Record suppliers may have assisted with system setup to include such software on managed terminals. NHS statistics suggest almost all pharmacies have already migrated onto newer browsers, but if there are any remaining pharmacy organisation (large pharmacy organisations as well as smaller ones) who have not done so yet, then migration plans can be implemented.
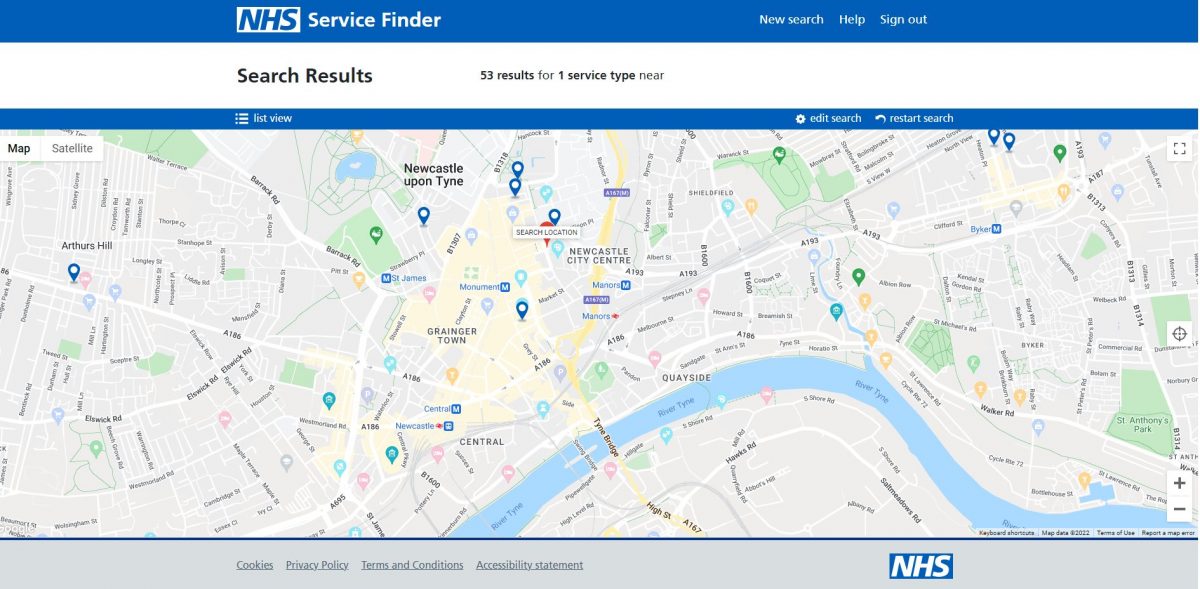
NHS Profile Manager
- Previously, community pharmacy teams used two different NHS systems to ensure their pharmacy details were up to date in the Directory of Services (DoS) and on the NHS website: the NHS website profile editor and the DoS Profile Updater. During late 2022, NHS Profile Manager launched to replace both the DoS Updater and the NHS website editor. Newer features within NHS Profile Manager mean you can now:
- update your facilities, e.g. confirmation of facilities such as car parking; and
- confirm whether you provide the NHS blood pressure check service and Pharmacy Contraception Service – within the service module.
- Community Pharmacy England published an NHS Profile Manager Spring 2023 reminder.
Next steps:
- NHS England’s Transformation Directorate continues to work with the pharmacy multiples regarding the NHS website and DoS Application programming interface (API).
- If pharmacy representatives wants to discuss the potential enhancements on the wishlist, please contact it@cpe.org.uk.
Other data security updates
- DHSC published a report on Cyber security strategy for health and social care: 2023 to 2030. This report set out how the government plans to achieve cyber resilience across the health care sector no later than 2030. Digital Health reported on this.
- NHS England’s cyber team said that:
- NHS England’s Transformation Directorate (NHS TD) patient safety team blogged that everyone working in health and care should protect the NHS from cyber-attacks, and that clear, supportive messaging will help people do their bit.
- Bennett Institute for Applied Data Science outlined why information governance is not enough when it comes to protecting privacy.
- Netskope Threat Labs has warned that threat actors are increasingly using cloud apps to target healthcare organisations with cloud malware delivery – rising from 38% to 42% in the past 12 months.
- Open Access Government reported that in order to establish an effective digital healthcare system, we need to build trust with privacy first, argues Nigel Jones, co-founder of the Privacy Compliance Hub.
Smartcard identity checking process to be digitized: Apply for Care ID
- Pharmacy team members must authenticate their identities to be linked to their Smartcards. Prior to the pandemic, pharmacy team members had to attend face-to-face meetings with local Registration Authority (RA) staff. The NHS implemented emergency policies throughout the pandemic so that staff could authenticate themselves remotely, e.g., via video calls. NHS England’s Transformation Directorate hopes that a successful early rollout will lead to the wider rollout of ‘Apply for Care ID’. This programme will enable health care staff use an NHS authenticator app as an alternative to a face-to-face visit to the RA. The service has incorporated feedback from Community Pharmacy England and CP ITG into their plans. The ‘Apply for Care ID’ online materials have been further updated since the last pharmacy IT bulletin.
Connectivity
- Digital Health reported that a new generation of 5G connectivity can unlock innovative approaches to treatment.
Pharmacy Show: Agenda re pharmacy IT
The Pharmacy Show has been the largest face-to-face gathering of pharmacy professionals during recent years. The next Pharmacy Show is scheduled for 15th-16th October 2023. It will include sessions regarding pharmacy IT.
IT policy: organisational changes and updates
- NHS England has plans to merge data with private healthcare institutions to process and share information on healthcare activity.
- NHS England and Health Education England have legally merged to create a new, single organisation to lead the NHS in England.
- NHS England’s digital chief Tim Ferris to leave in September.
- King’s Fund speakers opined that Digital transformation of the health service will only be successful if innovators feel free to experiment and those who control budgets are realistic about the timeline for change.
- DHSC was seeking a “key senior leader” to advise the health secretary on digital, data and innovation.
IT policy: Delivery plan for recovering access to primary care
- The Government and NHS today promised a £645m investment in community pharmacies over the next two years to support a pharmacy common conditions service, along with the NHS Pharmacy Contraception and NHS Hypertension Case-Finding services. The Delivery plan for recovering access to primary care referenced digital development:
“As part of the new funding and to ensure the highest standard of care for patients, we will invest to significantly improve the digital infrastructure between general practice and community pharmacy. NHS England will work with community pharmacy suppliers and general practice IT suppliers to develop and deliver interoperable digital solutions. These will streamline referrals, provide additional access to relevant clinical information from the GP record, and share structured updates quickly and efficiently following a pharmacy consultation back into the GP patient record. These IT improvements will improve existing and future services; for example, by allowing GP patient records to be updated following supply of oral contraception or a blood pressure consultation in community pharmacy.”
IT policy general updates
- The ‘key to the future of pharmacy IT’ infographic was updated following feedback from CP ITG and pharmacy members. Pharmacy members may provide further feedback to it@cpe.org.uk so that this infographic can be iterated as required.
- Community Pharmacy England published a roundup of Spring pharmacy IT developments.
- Pulse reported that the Government will digitise the NHS Health Check, which it said would ‘identify and prevent more cases of cardiovascular disease’.
- NHS Digital reported on engagement events and activities regarding NHS Spine development.
- HSJ reported that Microsoft’s roundtable of senior digital leaders found four focus areas that can help upscale the automation efforts in the NHS.
- NHS England published a report, Who Does What. This report aims to assist NHS England and integrated care system IT leaders to move forward together, following on from the commitments laid down in DHSC’s 2022 plan for digital health and social care.
- Practice Director of SCC Hyperscale, Damon Crawford, argues that three factors influence the SCC approach to working with NHS organisations on new solutions.
- BT published its annual report, Mind the gap: delivering digitally enabled change to the NHS. The related survey had asked NHS professionals to share their thoughts on digital transformation.
- GE Healthcare Europe shared views on the need for healthcare digitisation. It also outlined potential strategies for achieving digitation.
- Tunstall Healthcare opined on what the future may hold for connected solutions and digital health.
IT policy case studies: social care
- DHSC published guidance that sets out the government’s roadmap for transforming adult social care data in England.
- Digital Health reported on how the Government had been unable to meet its digital commitments to social care.
- PRSB and nursing representative Claire Sutton made the case for standardising digital social care records to help people live well for longer.
- Digital Social Care launched a guide to help Councils and social care providers avoid pitfalls when introducing new and emerging technology.
- County Councils Network published a report on Adopting the right technology to transform social care. The report looks into the impact of digital technology on adult social care, and the importance of implementing digital change across the care landscape.
IT policy case studies: GP and urgent treatment centres
- Dr Shanker Vijay, GP and Digital First Lead for London, explained why he was championing the national ‘Register with a GP surgery’ service and talks about improvements to the service.
- Dan Wintercross, Programme Director GP IT Futures at NHS Digital, explained the benefits of getting involved with the early adopter programme, which is giving GP practices the opportunity to shape the future of digital, data and technology in primary care.
- Digital Health reported that the shares in digital health firm Babylon Health fell sharply on news that the company is to be taken private as part of a new debt plan.
- RCGP published: Fit for the Future: GP Pressures 2023.
- BMJ opined on How can we improve the quality of data collected in general practice?
- Loughborough Urgent Treatment Centre will use the eTriage system from eConsult in a bid to tackle lengthy queues.
IT policy case studies: Secondary care
- NHS England plans to create 3,000 additional ‘virtual ward beds’ this year.
- NHS Digital launched a consultation on sharing data from private hospitals with NHS.
- Health strategist Sarah McGovern said that medication administration incidents have significantly reduced following the go live of an electronic patient record at the largest trust in the UK.
- NHS England is making a dynamic purchasing system its approved procurement route for trusts buying equipment and systems to run virtual wards and remote monitoring programmes.
- NHS Providers published a guide on effectively embedding digital in your trust.
NHS use of big data to support patient care and clinical research
- Boots UK managing director Sebastian James said that innovative data sharing between the NHS and community pharmacy could deliver a huge leap forward in early prevention of disease and improved management of long-term conditions.
- Forbes reported on the NHS Federated Data Platform, which aims to bring all the data handled by the NHS together into a single source where it can be used to improve decision-making and patient outcomes.
- Digital Health published reports on:
- Institute for Government outlined Government data sharing during the pandemic – the benefits and what enabled the change to practices and behaviours.
- Forbes reported on the building of the NHS Federated Data Platform – arguably the world’s largest healthcare data platform.
- The non-profit legal advocacy group Foxglove flagged upcoming challenges with managing procurement and information governance risks during the selection process for the provider of NHS England’s Federated Data Platform (the incumbent was Palantir).
Artificial Intelligence (AI)
- Pharmaceutical Journal reported on datasets of patient data and AI replacing clinical decision support rules.
- Microsoft said that innovative technologies powered by AI can boost NHS productivity and help it recover from the pandemic.
- The Secretary of State for Health and Social Care says the UK government’s investments in AI can help show the value of new technologies while accelerating their use in the NHS.
- The Government launched a white paper on the use of AI, to drive responsible innovation and maintain public trust in this revolutionary technology.
- Medical Futurist reported on a Physician’s visual guide to AI.
- NHS England has launched an AI and digital regulations service for health and social care.
- Mirage reported on a new AI software that can help to spot prostate cancer is being trialled by researchers at Oxford University Hospitals NHS Foundation Trust.
- NHS England pilots AI software to cut missed hospital appointments.
- University of Manchester reported that AI and Digital Healthcare Technologies Capability framework published.
- The Health Foundation considered the opportunities and ramifications for AI use within health care.
- NHS England Transformation Directorate’s Director of AI said AI regulatory framework and workforce training are key AI priorities.
- Tech Monitor reported that many governments are reconsidering the effectiveness of their national AI strategies in light of recent strides in advancements amongst a string of AI technologies.
- NetApp’s Head of AI highlighted how beneficial the use of AI can be as a powerhouse tool of transformation in the health care industry.
- Digital Heath reported that AI-driven predictive analytics can help the heaviest users of health services to self-care and save the NHS from disaster.
- Information Age reported that OpenAI, the developer of ChatGPT, has enlisted UK start-up Faculty to help businesses generate new value opportunities with generative AI.
- A new regional NHS programme is using AI technology to identify high-risk patients on waiting lists to help reduce their risk of deterioration.
IT policy: priorities, reports and the future
- Global Legal Group published a report: Digital health laws and regulations: emerging trends in the global regulation of digital health – 2023.
IT policy (local): Integrated Care Systems
- The Rt Hon Patricia Hewitt was commissioned to lead an independent review of integrated care systems in November 2022. The report was published in spring 2023: The Hewitt Review: an independent review of integrated care systems. Members of the health tech industry shared views on Patricia Hewitt’s review of ICSs.
- More than half of ICSs reportedly lacked ‘crucial’ health management systems.
- West Country ICS introduced new ‘intelligent care traffic control centres’, using AI technology intended to visualise current healthcare demand, capacity and to predict future need.
- NHS Confederation reported on Tom Loosemore and Deborah El-Sayed exploring how integrated care boards can capitalise on the digital revolution.
- Bedfordshire, Luton and Milton Keynes Integrated Care Board has rolled out new technology across its websites to help make information about health and care services easier to access.
- DrDoctor, the patient engagement solution secured £10 million of investment to advance its plans for delivering patient-initiated models of care to integrated care systems.
- HSJ reported on their recent Digital Transformation Summit, where board representatives from ICS and provider organisations discussed the most pressing issues confronting digital health leaders.
- East of England Ambulance Service NHS Trust is to become the first ambulance service to pilot new technology that provides robust connectivity for ambulance crews and vehicles, even in areas where cellular connectivity is impossible.
Digital inclusion
- Electronic Immigration Network reported on how digital exclusion negatively impacts the health and well-being of asylum seekers.
- National Voices published a report on Tackling inequality and disadvantage: Key actions policy makers, commissioners and provider organisations can take when developing an approach with a digital component.
- The King’s Fund explored moving from exclusion to inclusion in digital health and care.
Innovation
Digital capabilities
- Health Education England (HEE) conducted a review looking at the progress made on recommendations from the 2019 Topol Review.
- A BT study found that nearly three-quarters of NHS staff believe technology could help transform patient care in England, with more than 80 per cent claiming it could attract more ’digital natives’ into the workforce.
- TechHQ reported on the uptake of digital technology within the health care sector.
- A research project finds connections within secondary care of connection between digital maturity and patient safety ratings.
- Imprivata launched two free tools: the Digital Identity Maturity Model and Digital Identity Maturity Assessment.
- Claire Read reported that NHS England’s new digital maturity assessment questionnaire can support valuable discussions about local priorities, one of those involved in the pilot has said.
- Digital Health Academy added a new foundation-level module that aims to bridge the engagement gap between health innovators and patients.
- BMC Medical Education published a study: Evaluation of the impact of technical physicians on improving individual patient care with technology.
- BCS Echo reported that pharmacists at Basildon Hospital were among the first to be trained using bespoke virtual reality technology.
Technology
- PocDoc expanded across Community Pharmacy (across 300 locations and four large community pharmacy chains ), powering digital Health Checks.
- NHS Digital described plans to modernise the NHS Spine platform and invited IT professionals to help shape its future.
- Consultant Connect opined that effective digital triaging and consultation programs hold the promise of shifting pressures from overburdened parts of the NHS such as general practice and A&E.
- NHS England Transformation Directorate’s cloud team said more NHS organisations should migrate to the cloud and explained the help available.
- The Chancellor of the Exchequer’s ‘budget for growth’ has laid out the UK government’s proposed road to making the country a ‘science superpower’. Over five years, £310m will be provided to continue facilitating digital health innovations for mental health, musculoskeletal and cardiovascular conditions. The implementation of such digital technologies is intended to alleviate pressures within the NHS.
- Medical Device Network reported that following news of proposed rule changes that will allow greater controlled-medication flexibility, telemedicine’s usage is reaching beyond the original pandemic-related framework.
- Sheffield University researchers found remote technologies help occupational therapists get patients home quicker.
- UK Parliament published a research briefing on medical technology regulations and the NHS.
- Tech Explore reported on Garmi a product of a new sector called geriatronics, a discipline that taps advanced technologies like robotics, IT and 3D technology for geriatrics, gerontology and nursing.
- Partner at global intellectual property firm Marks & Clerk, discussed the importance of medical technology and how efficiencies could be improved within the health sector.
- Med Tech reported on 3D printing within healthcare.
- Diginomica opined whether the Metaverse can be fit for purpose for optimal healthcare services?
- University of Cambridge researchers found that robots can help improve mental well-being at work—as long as they look right.
- MedTech reported on its FUTURES Conference which highlighted NHS’s need for technological solutions.
Culture
- The King’s Fund explored how Tech transformation disrupts leadership styles.
- NHS England’s digital workforce strategy team said that success for NHS is when the organisation is not using the word ‘digital’ and it instead becomes “a fundamental part of our DNA”.
- NHS Providers published new summary guidance on what makes a digital transformation a success. Digital Health reported on this.
Interoperability
- PRSB’s chief executive officer said that healthcare professionals are working flat out to provide care – which makes it the ‘perfect’ time to digitally transform services.
- Product Owner of the NHS API Developer Community, talked about how they’ve improved support for teams integrating with their products and services – and outlines their next steps.
- Hazel Jones from Made Tech discussed how to improve the adoption of open source in the NHS?
Booking and Referral Standards (BaRS) update
NHS England’s Transformation Directorate’s BaRS programme aims to enable booking and referral information to be sent between NHS service providers in a format useful to clinicians. The intention is that BaRS will eventually be available in all care settings. CP ITG feedback indicated that the BaRS programme should be expanded to incorporate NHS appointments standards.
Referrals & appointments updates
- Following the deployment of a specialist outpatient scheduling system, Leeds Children’s Hospital has delivered more than 1,700 additional outpatient department clinics.
- NHS England launched a campaign to encourage all acute trusts to give patients the ability to make appointments and receive messages online.
- NHS Digital explained why they’ve put sustainability into the NHS digital design principles.
- Kelly Calvert, health strategist explained why supporting efficient workflows is essential in the deployment of medical devices.
See: CP ITG workstream updates (archive) for older updates in html format. The bulletins (including the most recent one) can also be downloaded in pdf format at the CP ITG webpage.
Get involved
If you have a related query or would like to feed into the CP ITG or share your updates about IT and digital issues then please don’t hesitate to contact one of the group’s organisers, Dan Ah-Thion or it@cpe.org.uk or you can also sign-up to join the virtual Community Pharmacy Digital Group which helps inform CP ITG’s work with others. You can be involved as much or as little as you like with CPDG, and can unsubscribe from that email group at any time.
Return to the Pharmacy IT hub; CP ITG; Get involved; IT policy or IT a-z index