Choosing/changing a system supplier
Published on: 10th September 2014 | Updated on: 29th January 2024
Pharmacy systems are business-critical so consider carefully your options when selecting suitable system suppliers, with the features you will need now and in the future for relevant services
Additional questions that you may want to discuss with your existing or prospective supplier include:
- Features: Does the system have those frequently requested features that you’d want? Does it have the features listed within the Community Pharmacy IT Group’s (CP ITG‘s) Wishlist of system features? What current does the system have? How does the supplier provide enhancements beyond the minimum standards?
- Interfaces and efficiency: How effectively does the supplier and its interfaces support efficient working?
- Service level performance: Do they accept emails, and respond or resolve within an adequate service level agreement timescale? What are the guaranteed response times for dealing with problems when they occur? What are the escalation routes if the supplier doesn’t meet the guaranteed response times? Are there options available for raising an incident or do all support requests need to be made by phone? What are the helpdesk opening hours? Etc. (See also: one-page briefing about IT escalation).
- Innovation: Does the supplier publish its future roadmap, and welcome feedback for this. Does it innovate learning from technical developments occurring from within and outside of health and care? Does it have a method to genuinely take on board requests for future enhancement from its customers?
- Data provision: Does the supplier share relevant summary data (anonymised where appropriate) to relevant parties which might include the pharmacy, the commsionner, LPCs and NHS England – as needed to support ongoing community pharmacy service provision?
- Pricing: What upfront and ongoing costs are associated with use of the tools? What costs will be incurred in upgrading (one-off and ongoing)? Keep in mind that system suppliers also require viable business models, to prevent them needing to close down, and if they are going to seek to provide adequate systems and support
- Contract Length: What is the contract length and the detail of the service level agreement? Can the payment be associated with your prescription or service volumes? Is there a penalty clause for early termination of the contract? What is the ease and cost of transferring data into the system at the beginning of the contract or out of the system at the end of the contract? Contracts with a long duration period are not recommended.
- Additional hardware? Will the pharmacy need any additional hardware? Will this be provided by the system supplier or will you have to purchase it separately?
- Connectivity, router quality and replacement cycles: Routers have been identified as one of the key factors which enable better internet speeds. What are the arrangements for replacement cycles so your hardware is always up-to-date (see cpe.org.uk/routers, cpe.org.uk/hscn and getting the most out of your connections and connection arrangements)?
- Failures and contingencies: What arrangements are in place for when something goes wrong? What contingency arrangements are put in place to ensure that there is business continuity, for example 4G back-up cards, off-site back-ups etc.?
- Training at start: How does the system supplier plan to train pharmacy staff in using the new system? Is refresher training available if there is a gap between installation and system use? What type of training is being offered and does it meet the needs of your pharmacy team?
- Ongoing support: What ongoing system support is available?
- User-testing? How much user engagement is there in the ongoing development of the system? Are you able to feed in to support continued development and improvement?
If it is an EPS system specifically, consider:
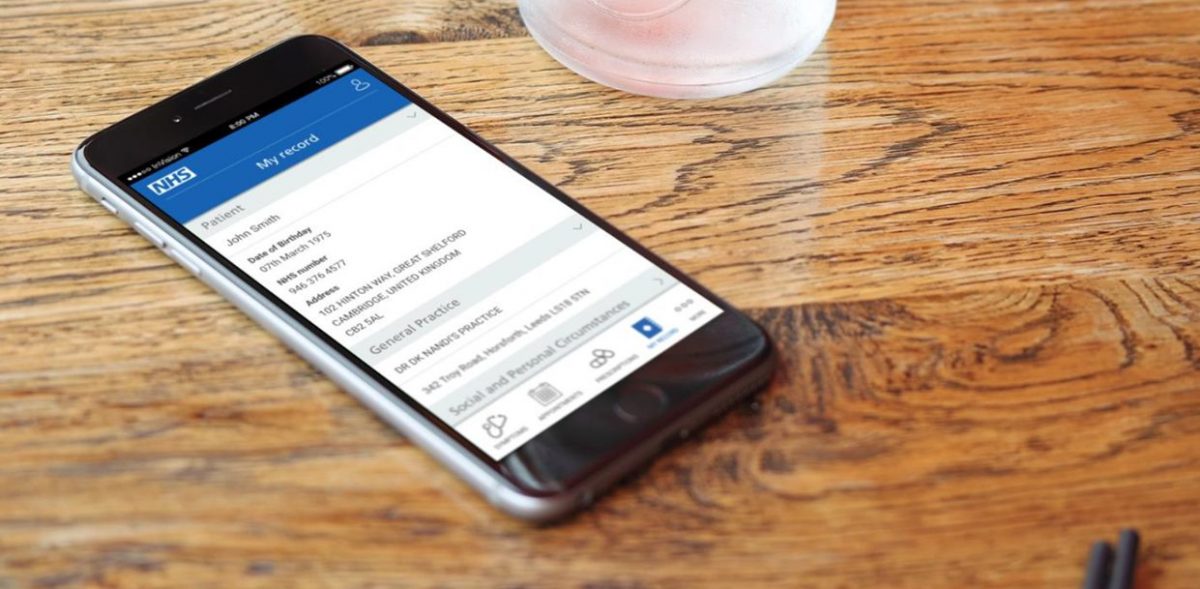
- Beyond EPS: What functionality is in the system or in development to support the provision of services (for example support for the New Medicine Service, support for recording MURs electronically and generating printed copies of the MUR Form etc.)?
- Robot/other integration? If the pharmacy uses or is planning to use an electronic point of sale (EPOS) system or dispensing robot or another integration, does the systems integrate with this technology.
- Alerts and reports: How effectively will the system alert you to issues, or prescriptions which haven’t been claimed? What type of reports will the system be able to generate, i.e. your end of month figures to include in your submission document to the NHSBSA? Or, identifying patients who have incomplete exemption status?
- ODS code change: after there has been a change of ODS code at a pharmacy, how this could impact how NHS IT such as EPS will function within the pharmacy. See ODS Codes.
For a CPCF services IT system:
- Can the system show the number of service reports submitted to the NHSBSA monthly? This would help you to compare the service delivery totals with the totals that are received into the NHSBSA’s MYS system.
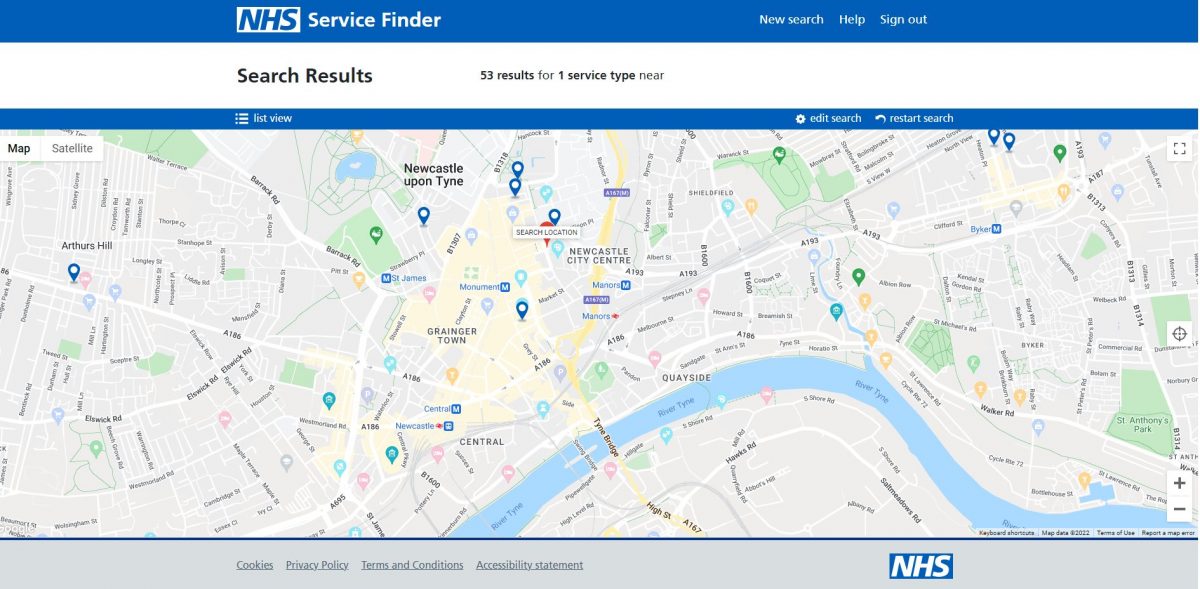
A range of organisations are involved with setting out and implementing IT policies at the local level.
As a principle, Community Pharmacy England and Community Pharmacy IT Group pharmacy representatives have supported the principle of LPCs, Integrated Care Systems, Local Authorities and local commissioners supporting local IT projects consider:
“To foster a robust and competitive environment, local standards, frameworks, and tenders should be designed to accommodate a wide range of IT system suppliers. Doing so creates a healthier marketplace that is more appealing to vendors. These vibrant marketplaces promote competition across various dimensions, including features, innovation, service levels, data provision, pricing, interoperability (alignment to NHS IT and other standards) and overall value to healthcare teams (such as pharmacy and GP practice teams) and taxpayers.
Rather than fixating on a single solution within a larger IT ecosystem, localities (as well as national policy teams) are encouraged to embrace a diverse array of suppliers or look towards lists with a multitude of assured suppliers that meet relevant criteria. This approach benefits healthcare teams (such as pharmacy teams), and their patients across the longer term and contributes towards a more dynamic IT landscape.”
- Suppliers and pharmacy contractors should consider avoiding long contracts (e.g. above a maximum one year in time) because of the associated inflexibility for all parties.
Refer to the ODS/IT change checklist which deals with both ODS/IT and supplier change: IT and ODS change checklist
Note that minimum timescales may be required to change systems. For example change of CPCF service DoS profiling may require at least ten working days. Your outgoing and incoming supplier should also be able to advise on timescales. There are recommended timescales for PMR system suppliers to use during system change – see the documents within the section below about “Process for PMR data transfer”.
Community Pharmacy IT Group (CP ITG) previously supported developing a recommended minimum dataset for cases where a pharmacy contractor has switched from one PMR system to another. For the sake of continuity of patient care, it is critical for some patient information to be transferred from the old to the new system.
Community Pharmacy England has worked with a CP ITG sub-group on a minimum dataset and associated transfer specification document:
Pharmacy patient IT system transfer (CP ITG specification)
CP ITG Pharmacy IT system transfer spec (Appendix 1 – dataset)
This was updated in June 2023 to a version 1.0, taking into account of system supplier comments.
The ‘latest start date for use of this specification’ is 1st October 2024, although suppliers should use it before this time wherever possible.
See also:
- Pharmacy system: requested features and development
- System specifications
- List of system suppliers and their contact details
- Reporting or feeding back about IT issues
If you have queries on this webpage, or wish to suggest possible spec changes (in case of future amendment opportunities) or you require more information, please contact it@cpe.org.uk. To share and hear views about digital developments with like-minded pharmacy team members, join the CP Digital email group today.
Return to the Pharmacy IT hub; System suppliers or IT a-z index