What does the patient pay?
Published on: 18th June 2013 | Updated on: 3rd May 2024
The Department of Health and Social Care (DHSC) uplifted the NHS prescription charge to £9.90 from 1st May 2024.
The NHS prescription charge is reviewed annually.
Community Pharmacy England has designed a downloadable Prescription Charge Card for community pharmacies. As well as a printable colour PDF, we have also provided a version optimised for printing in black-and-white.
Both versions have been designed to be easy to download and print ready for display in community pharmacies.
Prescription Charge Card 2024/25 (colour)
Prescription Charge Card 2024/25 (black and white)
Please note we revised our Prescription Charge Card on 2nd May.
Prescription Prepayment Certificate
Prescription pre-payment certificates (PPCs) offer savings for those needing four or more items in 3 months or more than 12 items in one year.
There are 3 PPC options to choose from:
- 3-month PPC costs £32.05
- 12-month PPC costs £114.50
- 12-month Hormone Replacement Therapy (HRT) PPC costs £19.80
Community Pharmacy England has designed a downloadable prepayment certificate poster for community pharmacies. As well as a printable colour PDF, we have also provided a version optimised for printing in black-and-white.
Both versions have been designed to be easy to download and print ready for display in community pharmacies.
PPC Poster 2024/25 (black and white)
Further information for patients can be found here
What if the patient isn’t sure if they pay for their prescriptions or are exempt?
If a patient is unsure whether they pay for their prescription or they are entitled to free prescriptions, pharmacy staff should advise the patient to pay for their prescription and provide them with an FP57 Refund form with information on how to claim a refund at a later date.
Patients can read more about the NHSBSA check before you tick campaign here and check their exemption status using this tool.
Further information can be found on our website here
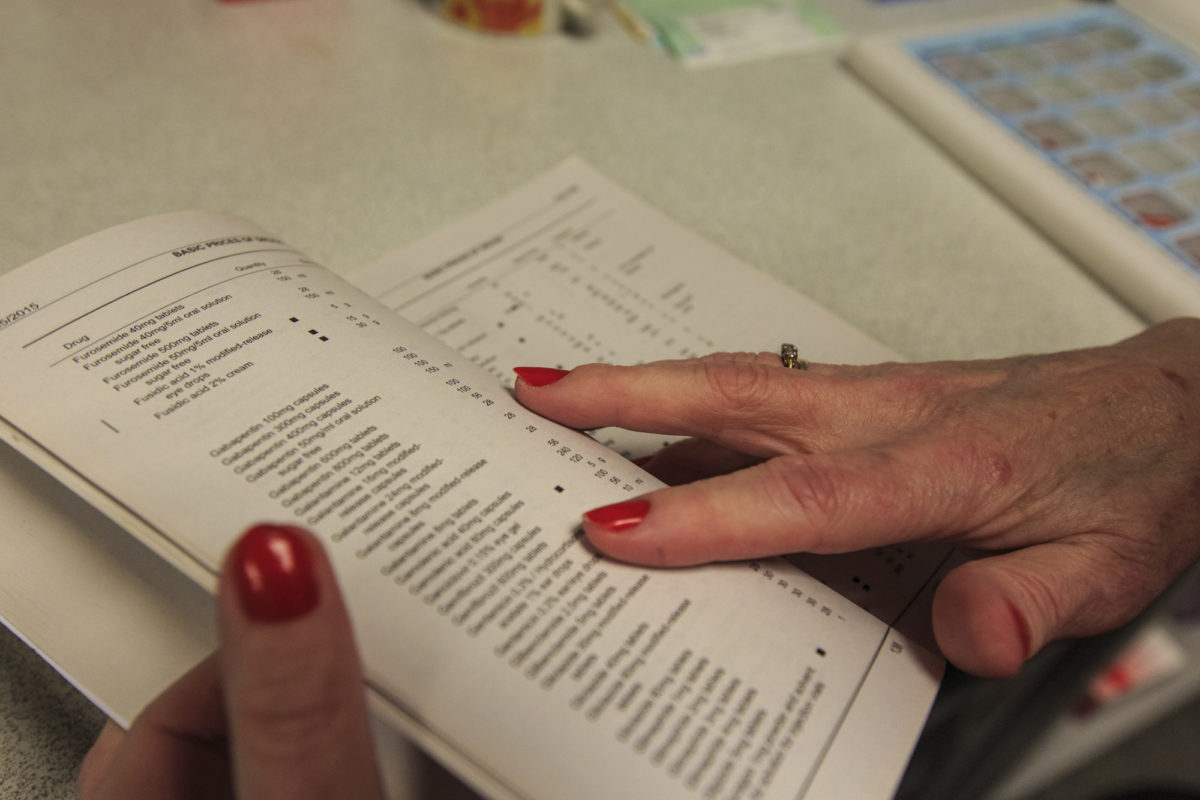
Part XVI of the Drug Tariff (Notes on Charges) sets out the categories of people who are entitled to exemption or remission from the prescription charge.
For information on patient eligibility of exemptions from prescription charges please see our page Exemptions from the prescription charge.
You may also wish to visit, or direct patients, to the NHS Help with Health Costs website: www.nhs.uk/healthcosts
When should you collect a prescription charge?
English pharmacy |
Welsh pharmacy |
|
| English prescription |
Collect prescription charges according to English rules |
Collect prescription charges according to English rules, unless the patient also presents a Welsh prescription charge entitlement card |
| Welsh prescription | Collect prescription charges according to English rules |
No prescription charges |
| Scottish prescription | Collect prescription charges according to English rules | No prescription charges |
| Northern Irish prescription |
No prescription charges |
No prescription charges |
Note: Only some prescription types are allowed to be dispensed in England click here for the full list.
Unless the patient claims an exemption, the following rules apply to determine how many prescription charges are payable.
Scenarios where a single prescription charge applies
Scenario |
Example of ONE charge (if written on same prescription) |
| The same drug or preparation is requested to be supplied in multiple containers. | Chloramphenicol 0.5% eye drops 10ml x 2 |
| Different strengths of the same formulation of a drug. |
Warfarin 1mg tablets x 28 Warfarin 3mg tablets x 28 Warfarin 5mg tablets x 28 |
| More than one appliance of the same type and specification (other than elastic compression hosiery). |
Open-Wove bandages 1 x 2.5cm Open-Wove bandages 1 x 5cm Open-Wove bandages 1 x 7.5cm |
| A set of different components making up a complete appliance. | Activa Leg Ulcer Hosiery Kit |
| Drugs in a powder form prescribed with a separate diluent (e.g. water for injections). |
Amoxil 500mg powder for injection x 1 Water for injection 5ml ampoules x 1 |
| A drug which needs to be supplied with a dropper, throat brush or vaginal applicator. |
Estriol 0.01% cream Vaginal applicator type 1 |
| Several flavours of the same preparation. |
Ensure Plus Fibre liquid banana Ensure Plus Fibre liquid strawberry |
| A medicine which is supplied with an appliance which is not listed in Part IX but is necessary for the drug’s use (see Part XVI, Clause 12.11, Drugs Packed with Non Drug Tariff Appliances). |
Emla 5% cream 5g + 2 dressings (previously known as the “pre-medication pack”) |
Scenarios where multiple prescription charges apply
Scenario |
Example of TWO charges |
| Different drugs, types of dressings or appliances prescribed on the same precsription. |
Absorbent lint BPC 25g Absorbent cotton BP 1988 25g |
| Different formulations or presentations of the same drug. |
Prednisolone 1mg tablets Prednisolone 2.5mg gastro-resistant tablets |
| Additional components supplied together with a complete set of apparatus or additional dressing(s) together with a dressing pack. |
Dressit sterile dressing pack Crepe bandage 1 x 7.5cm |
| More than one piece of elastic compression hosiery (anklet, legging, knee cap, below knee, above knee or thigh stocking). | 1 pair Thigh Stockings – Class II Black |
Bulk prescriptions
Part XVI, Clause 9 of the Drug Tariff sets out the arrangements for Bulk prescriptions
No prescription charge is payable when a bulk prescription is dispensed.
For further details on Bulk prescriptions see our page Is this prescription form valid?
Contraceptives
Part XVI, Clause 10 of the Drug Tariff sets out the arrangements for charging of contraceptives.
Prescriptions for the following items are automatically exempt from prescription charges:
- spermicidal gels, creams, films and aerosols
- systemic contraceptive preparations listed in Part XVI
- contraceptive devices listed in Part IXA of the Drug Tariff.
However, there are some products, such as Co-cyprindiol 2000mcg/35mcg tablets, which whilst they do not appear in Part XVI, are sometimes used for contraceptive purposes. In this scenario, if the doctor has endorsed the prescription with “CC”, “OC” or the female symbol (♀) to make it clear that the item is for contraceptive use, the patient should not incur a prescription charge.
Drugs packaged with non-Drug Tariff appliances
Sometimes, such as with Emla 5% cream, a drug is available packaged with items which are appliances that would not normally be allowed on an FP10 prescription because they do not appear in Part IX of the Drug Tariff. These “Non Drug-Tariff Appliances” are only permitted because they are packed with a prescribable drug and are required as part of the drug’s use. Contractors should be aware that the patient would pay just one prescription charge (and the pharmacist would receive only one fee) because the charge is related to the prescribable drug only.
More information is available in Part XVI of the Drug Tariff (Clause 10.11 Drugs Packed with Non Drug Tariff Appliances.)
Elastic hosiery
Multiple charges apply where more than one piece of elastic compression hosiery (anklet, legging, knee cap, below knee, above knee or thigh stocking) are ordered.
Prescription charges for elastic hosiery are calculated per garment (e.g 2 pairs of stockings = 4 garments) but professional fees are calculated per prescription item (e.g 2 pairs of stockings = 1 prescription item). Therefore two pairs of stockings would incur four patient charges and the pharmacy contractor would receive one professional fee.
Lymphoedema garments
Only one prescription charge is payable if the base garments or compression sizes are the same (i.e. both open toe or both class 1). If the size (i.e. S, M, L, XL or I, II, III, IV, V) or length (i.e. standard, petite, short or long – not below knee or thigh high) or colour is different, this would still be one prescription charge regardless of quantity.
Multiple prescription charges for lymphoedema garments apply where completely different base garments (i.e. open toe and closed toe or knee high and thigh high) or the same garment of differing compression sizes (i.e. Class 1, Class 2) are ordered.
Optional extras are classed as no charge items. No additional fees or charges are payable because all that is being dispensed is the base garment with optional modifications.
Multiple dispensing fees (Single Activity Fee)
If on an FP10 prescription there is a request for mixed, assorted or various flavours and the pharmacy contractor endorses to show that several flavours of the same preparation are supplied, they will receive a number of fees equivalent to the number of different flavours supplied. The patient will pay just one charge regardless of how many flavours have been dispensed. If the prescription does not state mixed, assorted or various flavours, only one fee will be paid regardless of whether multiple flavours have been dispensed or endorsed.
For more information on prescriptions requesting multiple flavours see our Multiple flavours factsheet
The NHS Business Services Authority (NHSBSA) have also confirmed that when different colours of the same preparation are prescribed on the same prescription form, only one prescription charge should be levied. The pharmacy contractor will receive one dispensing fee for each prescribed colour of the preparation supplied to the patient.
Q. I have received an FP10 Prescription for two pairs of ‘compression hosiery class II thigh length stocking circular knit standard stock size’; how many prescription charges should the patient pay and how many fees can I claim?
Multiple charges apply where more than one piece of elastic compression hosiery (anklet, legging, kneecap, below knee, above knee or thigh length stockings) are ordered. Prescription charges for elastic compression hosiery are calculated per piece of elastic hosiery. Two pairs of compression hosiery = four pieces and this would attract four charges from patients who usually pay for their prescriptions. Note different rules for charges apply to lymphoedema garments.
Professional fees for elastic compression hosiery are calculated per prescription item – two pairs of compression hosiery = 1 prescription item. As this prescription is for 1 item you would receive one single activity fee.
Q. How are prescription charges and fees calculated for lymphoedema garments?
Only one prescription charge is payable where one or more of the same lymphoedema base garment is supplied. For example, if a prescription orders multiple sizes (i.e. S, M, L, XL or I, II, III, IV, V), lengths (i.e. standard, petite, short or long – not below knee or thigh length) or colours of the same base garment it would only attract one prescription charge and one single activity fee regardless of quantity ordered.
Multiple prescription charges and fees would only apply where completely different base garments (i.e. open toe and closed toe or thigh length and below knee) or the same lymphoedema garment of differing compression sizes (i.e. Class II and Class III) are ordered.
Some lymphoedema base garments can be ordered with ‘additional options’ or optional extras. Additional options are classed as no charge items and therefore do not incur additional prescription charges nor do they attract additional prescription fees; however pharmacies are reimbursed for the cost of the optional extra.
Q. How many charges should a patient pay for a single item on an FP10MDA with multiple instalments?
Only one patient charge applies where the same drug or formulation is being dispensed; patients do not pay a separate prescription charge for each instalment dispensed.
Q. How many charges should be levied for multiple flavours of a preparation ordered on a prescription?
If the patient pays for their prescriptions, they would only pay a single prescription charge for a prescription ordering multiple flavours of the same preparation.
Q. I have received an FP10 prescription for a Nicorette inhalator starter pack and refill pack, how many prescription charges should the patient pay?
The patient would pay only one prescription charge (and the pharmacist would receive only one fee) as the same drug has been prescribed twice. The inhalator itself is a “non-Drug Tariff appliance” but is allowed because it is packed with the drug (Nicotine inhalator cartridge) and is required to enable the patient to take the medicine. More information is available in Part XVI of the Drug Tariff (Clause 10.11 Drugs Packed with Non Drug Tariff Appliances.)
Q. How many prescription charges should be levied if both carbamazepine 200mg tablets and carbamazepine MR 200mg tablets are prescribed on the same FP10 prescription?
Where different formulations or presentations of the same drug or preparation are prescribed and supplied, multiple prescription charges are payable (see Part XVI, Clause 11.2 of the Drug Tariff). In this example, as standard tablets and modified-release tablets are different formulations, two prescription charges would be payable unless the patient was entitled to exemption or remission from the charge
Q. I have a prescription requesting both Paroxetine 20mg tablets and Seroxat 20mg tablets, how many patient charges do I collect?
One patient charge should be collected as both items are the same generic drug and the same formulation.
The NHSBSA does not differentiate between the generic name and brand name as they are both the same generic product.
Q. I have received an FP10 Prescription for two pairs of Thigh Stockings – Class 2. How many prescription charges should the patient pay and how many dispensing fees can I claim?
Prescription charges for elastic hosiery are calculated per garment (2 pairs of stockings = 4 garments) but professional fees are calculated per prescription item (2 pairs of stockings = 1 prescription item), therefore two pairs of stockings would incur four patient charges. The pharmacy contractor would receive one dispensing fee.
Note: -lymphoedema garments are not hosiery, and as such, where more than one lymphoedema garment of the same type is supplied, only one prescription charge should be levied. E.g. Jobst Elvarex Custom Fit Class 1 Thigh High Stockings would incur just one prescription charge.
Q. How many patient charges for two pairs of lymphoedema stockings prescribed on the same prescription but which are different classes and lengths?
As different classes and/or lengths of a lymphoedema garment are recognised as difference types, each type will attract a prescription charge. For example Mediven Elegance Class 1 Below Knee Closed Toe and Mediven Elegance Class 1 Thigh Closed Toe would attract two prescription charges in total.
Q. I have a prescription for Sigvaris Comfort class 1 below knee open toe normal and Sigvaris Comfort class 2 below knee open toe normal lymphoedema garments; how many prescription charges will apply?
Two prescription charges will apply.
Multiple prescription charges for lymphoedema garments apply where completely different base garments (i.e. open toe, closed toe) or the same garment of differing compression sizes (i.e. Class 1, Class 2) are ordered.
Only one prescription charge is payable if the base garments or compression sizes are the same (i.e. both open toe or both class 1). If the size (i.e. S, M, L, XL or I, II, III, IV, V) or length (i.e. standard, petite, short or long – not below knee or thigh high) or colour is different, this would still be one prescription charge regardless of quantity.
Q. If an optional extra is prescribed with a lymphoedema garment on the same prescription, will an extra prescription charge apply?
No, optional extras are classed as no charge items. No additional fees or charges are payable because all that is being dispensed is the base garment with optional modifications. For example: Jobskin MTM Premium class 2 armsleeve lymphoedema garment FP0501-2 = 1 patient charge and 1 dispensing fee. Reimbursement is made for both the base garment and the optional extra at the Drug Tariff list price.
Q. I have received an FP10 prescription for two pairs of Tubifast socks, how many prescription charges apply?
These products are considered to be “stockinettes” rather than “elastic hosiery” and are listed as such in Part IXA of the Drug Tariff. The general rule is that only one charge is payable when more than one appliance of the same type (other than elastic hosiery) is supplied. Therefore, a prescription asking for 2 pairs of Tubifast socks would attract just one prescription charge.
Q. I have a prescription for Emla 5% cream. There is a pack that comes with occlusive dressings, if I dispense this what will I be reimbursed?
To keep in line with the Dictionary of Medicines & Devices (dm+d) descriptions (which prescribers are encourage to do), prescriptions for this item should be written as either:
Emla 5% cream 25g + 12 dressings
OR
Emla 5% cream 5g + 2 dressings
However, if a prescription is written simply as “Emla 5% cream”, pharmacy contractors can still be reimbursed for dispensing any of the available pack sizes (including the dressings packs), as long as they endorse the prescription accordingly (using the descriptions given above).
Please note that the patient would pay just one prescription charge (and the pharmacist would receive only one fee) because the dressings are “Non Drug-Tariff Appliances” which are only permitted because they are packed with a prescribable drug and are required as part of the drug’s use. More information is available in Part XVI of the Drug Tariff (Clause 10.11 Drugs Packed with Non Drug Tariff Appliances.)
Q. How many dispensing fees will I receive for dispensing an FP10 prescription for Qlaira?
Qlaira is a combination product which contains 5 different types of tablet; as such a pharmacy contractor would receive 5 fees for dispensing this item against an NHS prescription. However as Qlaira is recognised as a contraceptive drug, an NHS prescription for this item would not incur a prescription charge.
Q. I have received an FP10MDA prescription for 14 days’ supply with a total of 12 collections of methadone. How many prescription charges would the patient have to pay?
This item would incur just one patient charge. Part XVI, Clause 11.1.1 of the Drug Tariff states that a single prescription charge is payable where “the same drug or preparation is supplied in more than one container” and this is what is being requested on the FP10MDA prescription. More information on instalment dispensing can be found on this page of our website.
Q. A patient has presented one FP10 prescription for Sertraline 50mg tablets and another separate FP10 for Sertraline 100mg tablets. How many charges does the patient pay?
The patient would pay 2 prescription charges. This is because the medicines are on two different prescriptions and therefore each prescription incurs a patient charge.
Further “how many charges” examples can be found in Part XVI, Clause 12 of the Drug Tariff.
Q. Do I need to display a notice about the NHS prescription charge?
Yes, it is part of the NHS Terms of Service to have an up to date notice about the NHS prescription charge displayed in the prescription reception area. For further information, please see the clinical governance premises approved particulars.
Q. If a prescription was dispensed before the 1st May but the patient didn’t collect it until after the 1st May, should the patient pay the old or the new prescription charge?
There is no national guidance on this issue so pharmacy staff will be required to exercise their professional judgement. Whatever the decision, pharmacy staff are advised to record the charge made and the reasons for doing so on the patient’s PMR record.
Q. I have a paper prescription for a patient who was 59 years old when their prescription was issued; however, the patient did not present their prescription at the pharmacy until they turned 60. Is the patient exempt from paying a prescription charge?
Yes, subject to the prescription still being within its legal period of validity for dispensing. The reverse of a prescription says that entitlement to prescription exemption is based on the patient’s circumstances on the day they are asked to pay. In this case, as the patient was over 60 years of age when they presented their prescription at the pharmacy for dispensing, he/she would therefore be exempt from paying a prescription charge. If the patient’s age on the front of the prescription is printed as “59”or the prescription is handwritten, the reverse of the paper FP10 must be signed and the relevant age exemption category ‘A’ on the back of the form should be marked to declare that the patient is indeed 60 years of age or over for entitlement to charge exemption.
Q. I have an electronic prescription for a patient who according to their date of birth was 59 years old when their prescription was issued; however, the prescription was not dispensed by pharmacy until they turned 60. Is the patient exempt from paying a prescription charge?
For electronic prescriptions, currently most dispensing systems auto-populate exemption category codes ‘A’ or ‘C’ based on the patient’s date of birth held in the EPS message. The selected EPS message code and the patient’s date of birth is included in the message transmitted to the NHSBSA which they use to determine a patient’s exempt or charge status. You can check the paid/exemption category currently applied onto an electronic prescription using your PMR system. However, the date the Dispense Notification (DN) message is submitted to the NHSBSA may be different to the date the patient was asked to pay, causing the need to override the exemption category auto-populated by the system. For further information on EPS exemptions, see cpe.org.uk/epsexemption
Q. Do patients pay prescription charges for SSP supplies?
Generally, prescription charges are payable for the supply of alternative products in accordance with SSPs, if they were payable for supply under the original prescription. The exception to this is that no prescription charge is payable if the patient is supplied with a smaller quantity of drug or fewer appliances than originally prescribed. This exception was proposed by Community Pharmacy England and accepted by DHSC Ministers in order that patients that pay the prescription charge are not disadvantaged by the use of an SSP.
Q. How many charges apply if the same item appears twice on a prescription?
One patient charge should be collected if the same item appears more than once on a prescription.
Q. How many charges apply when different pack sizes of the same drugs/appliances are ordered on the same prescription?
One patient charge should be collected if different pack sizes of the same drug/appliances appear on the same prescription.
Q. Is there a list of drugs to which the ‘FS’ prescriber endorsement can be applied to?
The ‘FS’ endorsement will operate by way of guidance; prescribers should exercise their clinical discretion in accordance with their professional duties and obligations.
For sexually transmitted diseases (STDs
There is no specific list of drugs to which the ‘FS’ prescriber endorsements can be applied to. It is considered that only those conditions for which sexual contact is a main route of transmission of an infection should be ordinarily managed as “STI treatment”, for example, treatment for chlamydia would be FOC whereas treatment for candidiasis would not. Guidance on STIs that may be suitable for managing in primary care can be found in the guidelines section of the BASHH website and in the standards for the management of sexually transmitted infections.
Free supply of certain COVID-19 trial medicines
There is no specific list of drugs to which the ‘FS’ prescriber endorsements can be applied to. The trial medicines are usually supplied directly to eligible participants by the clinical trial team. However, because some participants in these trials will be required to take the drugs for up to 12 months and the treatments are being used outside their normal licensed indications, the Medicines and Healthcare products Regulatory Agency (MHRA) have advised that GPs should prescribe the trial medicines to patients using an FP10 prescription form or the Electronic Prescription Service (EPS). The trial medicines used in HEAL-COVID are Apixaban and Atorvastatin. STIMULATE-ICP currently uses Famotidine and Loratadine (in combination), Rivaroxaban and Colchicine.
Q. How will the NHSBSA process prescriptions with ‘FS’ endorsed items?
The NHSBSA will recognise the ‘FS’ endorsement when it is correctly applied by the prescriber and treat the marked items as free-of-charge, accordingly.
In EPS, prescribers should confirm ‘FS’ by selecting the appropriate flag, so that the prescription carries the ‘FS’ endorsement correctly. The ‘FS’ endorsement must not be manually added by a prescriber to the free text field EPS dosage area or other free text sections of the prescription as this will not be recognised by the NHSBSA during processing. To ensure that ‘FS’-endorsed medicines are treated as FOC items by the NHSBSA, pharmacy teams must ensure the correct exemption reason is selected before the prescription is submitted for payment
On paper FP10’s, prescribers must endorse the front of the paper prescription form by writing ‘FS’ and signing next to each item. Paper prescriptions with items endorsed ‘FS’ should be placed in the red separator for exempt prescriptions when submitted to the NHSBSA for processing.
Q. How will prescribing systems accommodate this new change for electronic prescriptions?
The ‘FS’ endorsement has now been configured on prescribing systems for EPS. Prescribers should revert to issuing paper prescriptions with the ‘FS’ endorsement manually added against each item to be supplied FOC, if ‘FS’ isn’t working as expected.
Where configured into EPS, the message code ‘Y’ (0017) should be used for prescriptions containing only ‘FS’ endorsed items. The message code ‘Y’ (0017) should be populated before an EPS claim is submitted for payment (some PMR systems may automatically apply this code if an ‘FS’ endorsed item is prescribed).
Please note the ‘FS’ endorsement should NOT be manually added to the EPS dosage instructions field as this would not allow a pharmacy contractor to supply any item(s) FOC against NHS prescriptions. Addition of any free-typed supplementary information to the dosage instruction field or other fields such as ‘additional instructions’, will not be taken into account for reimbursement purposes as this information is not captured by the NHSBSA during processing. If an electronic prescription is received with the prescriber ‘FS’ endorsement contained within the dosage area, the prescriber should be contacted to cancel the prescription, and a correctly endorsed prescription re-issued. See cpe.org.uk/dosearea.
Q. Does removal of box X from the reverse mean that patients will now need to start paying for their contraceptives?
No. Contraceptives continue to remain free of charge (FOC) on NHS prescriptions. The removal of box X is because there is no requirement for patients to make a declaration to receive any FOC items against NHS prescriptions.
Q. Will the EPS message code ‘X’ (0010) for “was prescribed free-of-charge contraceptives” continue to remain available for selection in EPS?
Whilst category X is to be removed from the reverse of the new FP10 forms and Tokens, the EPS message code ‘X’ (0010) for “was prescribed free-of-charge contraceptives” will remain on EPS systems that usually display it. This message code remains on EPS systems because population of a message code field is mandatory before an EPS claim is submitted for payment to the NHSBSA.
Q. I received an EPS prescription for a contraceptive and inadvertently marked it as charge ‘paid’ when submitting the EPS claim message. Will a prescription charge be deducted by the NHSBSA during pricing?
Contraceptive drugs and appliances listed in the Drug Tariff (Parts IXA and Part XVI) and items endorsed ‘CC’ are automatically treated as FOC by the NHSBSA regardless of a patient’s exemption or charge status. So, if an EPS prescription for a contraceptive listed in the Drug Tariff (or item endorsed ‘CC’) is inadvertently marked as ‘paid’, no prescription charge will be deducted by the NHSBSA for these FOC items.
Q. If a prescription was dispensed before the 1 April but the patient does not collect items until after the 1 April, should the patient pay the old, or the new prescription charge rate?
There is no national guidance on this issue so pharmacy staff will be required to exercise their professional judgement. Whatever decision is taken, pharmacy staff are advised to keep a record of the amount charged and the reasons for doing so on the PMR. Please note the prescription charge rate is not determined by the date that the GP has prescribed or signed the prescription form.
Q. For EPS, how do the NHSBSA determine which prescription charge rate to apply if a paid prescription dispensed in April is submitted for payment in May?
Any paid electronic prescriptions dispensed in April 2024 with an NHS prescription charge levied at the old charge rate (£9.65) will have a charge deduction of £9.65 applied by the NHSBSA if the Dispense Notification (DN) message is submitted before 30 April 2024 and the corresponding Claim Notification or Electronic Reimbursement Endorsement Message (EREM) is received by the NHSBSA by the end of 5 May 2024. Please see below how paid electronic prescriptions are treated by the NHSBSA following a change to the prescription charge rate.
- If a DN is submitted on 30 April and EREM is received by NHSBSA by 5 May – this would be treated as April dispensing (£9.65 deducted for chargeable scripts)
- If a DN is submitted on 1 May and EREM is received by NHSBSA by 5 May – this would be treated as May dispensing (£9.90 deducted for chargeable scripts)
- If a DN is submitted on 30 April and EREM is received by NHSBSA on or after 6 May – this would be treated as May dispensing (£9.90 deducted for chargeable scripts). There would be no checking of the dispense date in this instance as the claim message was submitted would be outside of the first five days of the following month (EPS 5-day window).
Q. A patient has asked for a refund as they hold an exemption certificate but they were not provided with an FP57 form at the time of dispensing, how can they obtain a refund?
A prescription refund without an FP57 can only be considered in exceptional circumstances, if the patient believes this applies they should send proof of payment and a covering letter outlining the circumstances to:
Good Cause Reviewers
HES
NHSBSA Bridge House
152 Pilgrim Street
Newcastle upon Tyne
NE1 6SN
Email: nhsbsa.healthcostrefunds@nhs.net
Q. When should I submit details of any PPCs sold in March to ensure that the NHSBSA apply the correct rate deductions?
Pharmacies that are registered to sell PPCs should add and submit details of all PPCs sold in March 2021 on the PPC Pharmacy sales web application by 11.59pm on 31 March 2021 to ensure that the correct PPC rate deductions are applied by the NHSBSA.
Q. Where can I find the most up to date list of HRT medicines covered by the HRT PPC?
The list of HRT medicines covered by the HRT PPC will be published in Part XVI of the NHS Drug Tariff from April 2023. The up-to-date HRT medicines list will also be available on the HRT PPC application page and the NHSBSA help with health costs page.
Q. Can an HRT PPC be backdated?
Yes, the HRT PPC can be backdated by up to one month from the date of application (but not prior to 1 April 2023).
Q. Is the HRT PPC refundable?
The HRT PPC certificate is non-refundable, so patients must check this type of certificate is suitable for them before they purchase it. Patients can call 0300 330 2089 for help and support.
Q. Can a patient use the HRT PPC to claim exemption from charges for listed HRT medicines ordered on prescriptions issued prior to April 2023 but not dispensed until after April 2023?
Yes, the exemption applies from the date of dispensing.
Related resources
Factsheet: Free-of-charge (FOC) Items
Dispensing Factsheet: Exemptions from the prescription charge
Controlled Drug prescription forms and validity
Dispensing Factsheet: Checking Prescription Exemption Status
Dispensing Factsheet: New prescriber endorsement ‘FS’ for free supply of sexual health treatment
Exemptions from the prescription charge
Is this prescription form valid?
Prescription form section of the NHSBSA’s website (external)