Submitting EPS and eRD messages within time
Published on: 12th August 2014 | Updated on: 22nd August 2022
 Key information on EPS and timing is set out within the Claiming for EPS and eRD prescriptions on time factsheet.
Key information on EPS and timing is set out within the Claiming for EPS and eRD prescriptions on time factsheet.
On this webpage we explain how to reduce the risk of payment loss or delay caused by timing issues with electronic prescriptions.
SSPs timing information is also set out within FAQs below.
There are two key EPS notifications sent to the NHS Spine using your local patient medication record (PMR) system:
- Dispense notification (DN) message (or ‘dispense message’): This message is submitted once a prescription has been dispensed via EPS. Sending the dispense message may also be referred to as ‘dispensed’, ‘collected’ or ‘complete’ notification depending on the pharmacy system used.
- Claim notification (CN) message (or ‘claim message’): This is the final claim message that should be sent after the dispense message has been submitted by the pharmacy. The claim message includes endorsement information and information on the charge status of the prescription. The claim message may be referred to as ‘electronic reimbursement claim, ‘prescription claim message’, or similar depending on the PMR system used.
Example processes:
- Checking exemption status and endorsement prior to claim: Some pharmacy contractors may prefer that staff, for example locums, do not submit the ‘claim’ message at the same time as the ‘dispensed notification’ message to allow the contractor time to check that a prescription has been endorsed fully and appropriately before submission.
- Sorting by dispensed prescriptions to be claimed: Pharmacy systems may provide pharmacy staff with a list of electronic prescriptions which have not been submitted for reimbursement and which may be approaching the EPS 180-day limit, so that these can be completed and submitted when appropriate.
eRD (Electronic Repeat Dispensing) prescription issues must be claimed within 365 days of the prescriber’s original signature date because claim messages cannot be submitted beyond this point.
System suppliers have flexibility to introduce or improve the warnings and reports to alert pharmacies that prescriptions may go unclaimed because of the eRD 365-day limit.
This is a key area for contractors to discuss with their pharmacy system suppliers to ensure that systems meet the needs of pharmacy staff.
Example discussion points:
- What reports and alerts will be in place in the system to alert pharmacy staff of the need to claim these outstanding eRD batch issues when these are at risk of going unclaimed within 365 days?
- Will late eRD batch issues being processed close to the eRD 365-day limit cause extra warnings about the time limits?
See also the Tips section of this webpage (below), some of which relate to eRD time limits.
In these uncertain times where there could a risk of temporary closure of pharmacy businesses, Community Pharmacy England recommends that contractors consider the following top tips for EPS submission. Community Pharmacy England recommends that contractors should follw the below
We set out tips for the pharmacy team relating to timely EPS submission.
For EPS prescriptions:
- Claim messages should be sent to the NHS Business Services Authority (NHSBSA) no later than the 5th day of the month following that in which supply was made (Drug Tariff Part I, Clause 5A).
- Send dispense and claim messages frequently throughout the month. If all claim messages are submitted at the end of the month, there is a risk of delayed payments if a temporary closure or a technical issue prevents the successful transmission of claims. Send claim messages soon after the final dispense message has been sent, and before the 180-day (six month) limit . After 180 days, the prescription cannot be priced by NHSBSA.
- Urgently send claim messages where there are owings. All prescription items must be marked as either dispensed or not dispensed before you submit a claim message. If one of the prescribed items will be partially dispensed you can mark it that way, e.g. marking 14 of 28 tablets dispensed and the remaining tablets non-dispensed. Similarly, if a complete item is not required by the patient, the whole item needs to be marked as not dispensed, so that you are able to submit claim messages to claim for the other items dispensed on the prescription.
- Take into account the five EPS window explained further below.
For Electronic Repeat Dispensing (eRD) and EPS Controlled Drug (CD) prescriptions:
- Ensure that all eRD prescription issues are claimed within 365 days of the prescriber’s original signature date because claim messages cannot be submitted beyond this point.
- Ensure that CD (Schedule 2, 3 and 4) prescriptions are marked as dispensed, and claimed for in a timely manner. The law sets out that actual dispensing of the Schedule 2, 3 and 4 CDs must take place within 28 days of the appropriate date. Aim to ensure that any dispense messages and claim messages are sent within the same period. Your PMR system supplier can alert you of actual dispensing timelines but doesn’t need to prevent the dispense/claim messages being submitted after day 28 in case the actual dispensing took place within 28 days but the dispense/claim messages were sent later (e.g. a technical outage occurred on day 28).
Further tips:
- Submit claim messages to the NHS Business Services Authority (NHSBSA) no later than the 5th day of the month following that in which supply was made (Drug Tariff Part I, Clause 5A).
- Submit dispense and claim message frequently throughout the month (preferably daily). If all claim messages are submitted at the end of the month, there is a risk of delayed payments if unexpected pharmacy closure or a technical outage prevents the successful transmission of claims. In the event of a pharmacy closure this also allows other pharmacies, EPS users and the NHS to check the status of a prescription.
- Claim for any partially-dispensed items. All prescription items must be marked as either fully dispensed or not dispensed before you submit a claim notification messages. If a prescription has multiple items and one of the items is no longer required, by the patient, mark the item as ‘not-dispensed’ so that you are able to submit claim messages for any other items dispensed on the same prescription.
- Take into account the five-day EPS window to ensure dispense notification messages are sent within the calendar month and the corresponding claim messages are sent by the end of the 5th day of the following month
- Ensure that Schedule 2, 3 and 4 Controlled Drug prescriptions are marked as ‘dispensed’ and claimed for in a timely manner. The law sets out that actual dispensing of the Schedule 2, 3 and 4 CDs must take place within 28 days of the appropriate date.
- Ensure that all electronic Repeat Dispensing (eRD) prescriptions are claimed within 365 days of the prescriber’s original signature date because claim messages cannot be submitted beyond this point
- Claim soon after the final dispense messages have been sent, and before the 180-day (six months) prescription claiming deadline*. After 180 days, the prescription cannot be priced by NHSBSA.
Other PMR tips
To ensure your EPS prescriptions are sent on time consider how to:
- Filter and display prescriptions within your PMR system that still need dispense/claim messages to be sent.
- Learn how your PMR system alerts you of prescriptions marked dispensed approaching the 180-day EPS limit period but unclaimed; or downloaded but not marked as dispensed.
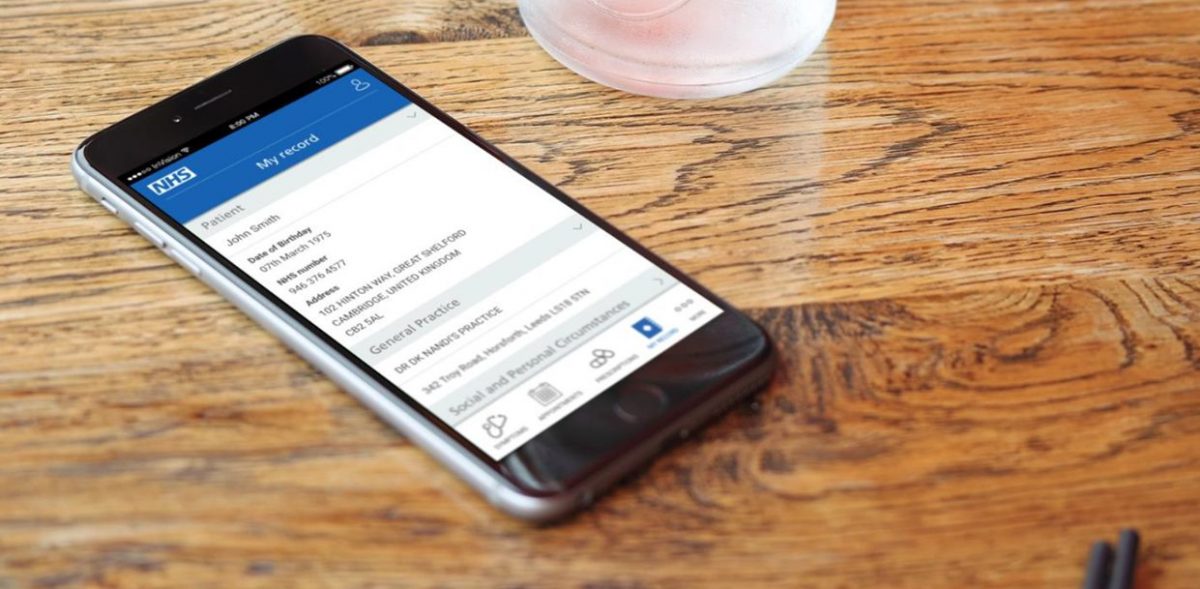
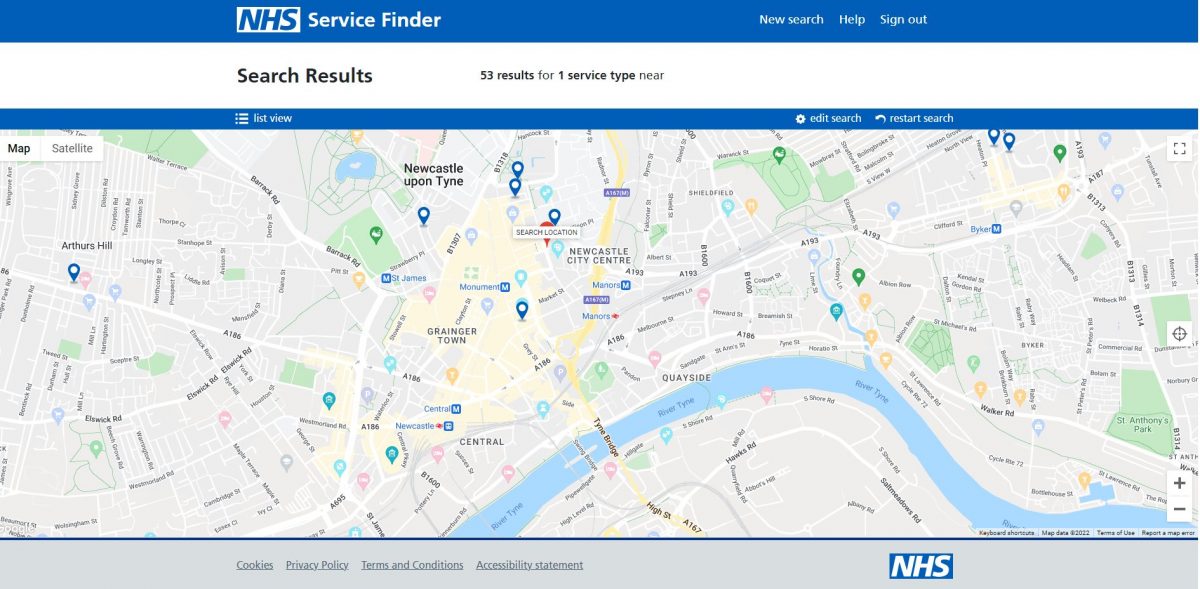
- Learn how to identify prescriptions which have not been submitted using the EPS Tracker which lets you enter a prescription ID or NHS number plus a date range. Read more at org.uk/tracker
- Use the claim amend feature if your PMR supplier has it if the 5th deadline has not passed. Deal with planned or unexpected system updates if these temporarily disrupt the sending of claim messages.
System suppliers have flexibility to introduce or improve the warnings and reports to alert pharmacies that prescriptions have gone unclaimed.
This is a key area for contractors to discuss with their pharmacy system suppliers to ensure that systems meet the needs of pharmacy staff.
Example discussion points:
- What reports and alerts will be in place in the system to alert pharmacy staff of the need to claim these outstanding prescriptions when these accidentally go unclaimed?
- Will there be a regular warning when logging in, advising that there are x number of prescriptions which were marked as dispensed more than three months ago but have not yet been claimed?
Read more at making your system work for you.
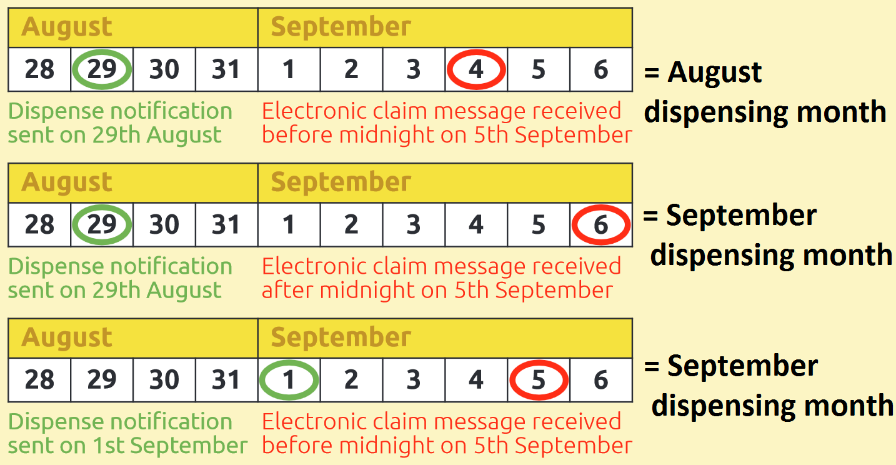
The dispensing month in which an EPS prescription is submitted and counted for payment is determined by two key dates: the dispense message date and the claim message date.
When a dispense message is sent before midnight on the last day of the dispensing calendar month, the claim message must be received by the NHSBSA before midnight on the 5th of the following month to be counted towards the total items for the actual dispensing month. However, if the claim message is submitted later than the 5th of the following month, the item will NOT be counted towards the actual dispensing month.
Tip: Submit dispense/claim messages in a timely manner because the prices paid for a medicine/appliance can vary from month to month, e.g. when a price concession in granted one month but not the next.
See examples below.
Following the explanation about the EPS 5-day window above, four scenarios outlined below explain how the timing of dispense and claim message submission can affect the timing of your payment.
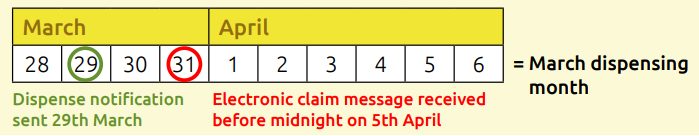
Scenario 1: Both dispense/claim message sent before the end of the dispensing month
The example shows a dispense message sent on 29th March and the claim message sent on 31st March. This claim will therefore be processed as part of the March dispensing month bundle.
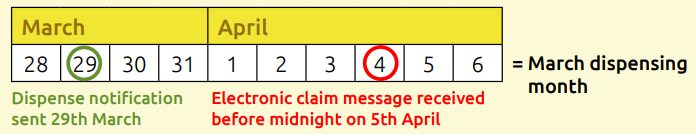
Scenario 2: Dispense message sent in dispensing month and claim message sent between days 1-5 of the following month
A dispense message was sent on 29th March and the claim message on 4th April (before the 5th April deadline). This claim will therefore be processed as part of the March dispensing month bundle.
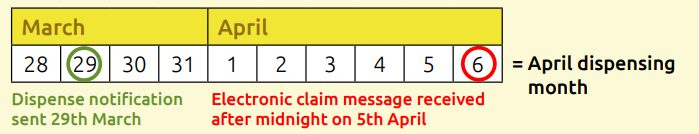
Scenario 3: Dispense message sent in dispensing month and claim message sent after day 5 of the following month
The example shows a dispense message submitted in March, but a claim message is sent on 6th April. This claim will therefore be processed as part of the April dispensing month bundle.
Scenario 4: Both dispense message and claim message sent between days 1-5 of the following month
Both the dispense message and claim message have been sent in the first five days of the month, so this prescription will be processed as part of that dispensing month (in this case, April).
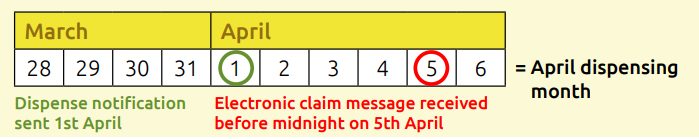
Note: For scenarios 3 and 4, these EPS prescription claims will NOT be included in your payment for prescriptions dispensed in March, even if it was inadvertently declared in your FP34C submission document for the March dispensing month bundle.
Examples of what might occur if all or part of an EPS prescription remains unclaimed are set out within scenarios A-D below:
Scenario A – Fully dispensed. No claim for 6 months
Prescription fully dispensed, but no ‘claim’ made within 180 days (six months) after the final dispense notification for an item. The prescription will pass its time limit but should remain visible on the local pharmacy system. Payment will not be made at the Pricing Authority (see Reimbursement for prescriptions passed deadlines below).
Scenario B – Partially dispensed. No claim for 6 months
Some items are marked as dispensed, but one item is left as partially dispensed and no claim is made within six months:
A prescription which has been left marked as partially-dispensed or owing will have its status changed to passing deadlines 6 months after the last dispensing event.
It is recommended you claim for what was dispensed rather than allowing a prescription to reach its time limit because part of it was not dispensed. Where needed mark an item or part of an item with “not dispensed” and submit your prescription
Scenario C – No items dispensed (and therefore no claim made) for 6 months
A prescription which is held on the Spine with no items dispensed for its 180 EPS time limit cannot have its dispense message sent. If dispensing is required, the patient should be referred back to the prescriber for a new prescription.
Patient requires further dispensing episodes against a script passed the 180-day EPS deadline
The patient should be referred to the prescriber so that a new prescription can be issued. (NB: The RPS issued guidance on the legal validity period for owing slips which depends on whether the prescription is for a Controlled Drug or not. Guidance on the legal validity period for owings differs from the 180-day EPS technical time limit caused by the Spine’s housekeeping rules to keep data on the spine manageable.)
Prescriptions will be held on the Spine for three months after 180 days with no processing allowed on these items. If an attempt is made to ‘pull down’ the item for dispensing, the pharmacy will be sent a rejection message informing the pharmacy staff that the prescription has passed its 180-day EPS time limit.
Reimbursement for a prescription passed 180-day time limit
After 180 days an electronic reimbursement claim to the NHSBSA could not be processed. A manual request (which may be based on an average) might be made to the local NHS England team who may speak with the Pricing Authority on the issue – if the issue was outside of contractor control.
Claim messages should be sent on time and the correct number of items declared on your FP34C submission document. PMR systems can generate reports showing the correct number of EPS and paper items to include on the FP34C. Do not count dispensing tokens when totalling EPS figures; use the reports generated by your PMR system.
A comparison could help you to identify if some prescriptions are not being claimed within time. Read more at: Process for checking EPS total item numbers (reconciling) factsheet
Q. I supplied a Serious Shortages Protocol (SSP) item within the SSP time period. Can I submit the SSP a bit late?
No, given that you should reduce the risk of non-reimbursement, by submitting SSPs both within SSP timeframes and within the relevant dispensing month bundle.
A scenario: If an SSP item was processed by you on the last day of the calendar month and this date also corresponded with the last day of the SSP arrangements being in place for this item, you should consider how to get your SSP item submitted within time. For paper prescriptions, you must submit it within the relevant dispensing month bundle. For an EPS prescription in this ‘late’ scenario, there are two options (EPS SSP method or EPS token SSP method) but the EPS token SSP method may be more suitable for you for taking into account points such as those covered below.
EPS Option 1 for scenario above: EPS token SSP method: You may decide to use the EPS token method instead of the EPS SSP method in scenarios in which there is risk that use of the EPS SSP method may put timely submission at risk. The EPS token should be submitted with the relevant EPS bundle being posted to NHSBSA.
EPS Option 2 for scenario above: EPS SSP method and issues to consider: If considering use of the EPS SSP method, you should take into account the EPS 5 day window and EPS submission timing. If you were unable to get the EPS form dispense message submitted in time for the last day of the calendar month (e.g. because of a computer outage or for another reason) and therefore the EPS dispense message could only be submitted within the next dispensing month at the earliest (causing a late submission of the SSP item via the EPS SSP method) then the EPS token method will need to be used instead and the token submitted with the correct dispensing bundle posted to the NHSBSA.
Q. I have a prescription with both an SSP item plus a non-SSP item. What if an owing delays the submission of the prescription and this might impact me submitting the SSP in a timely way? How do I handle such prescriptions?
It is for the contractor taking into account and their chosen systems and processes to determine when to send EPS messages. However, note the FAQ above relating to late SSP submission. See also EPS and submitting on time.
If you have a prescription with both an SSP item as well as another item where you plan to process the non-SSP item at a later date, you may want to consider using the SSP EPS token method instead of the EPS SSP method, if this will make it easier for you to get the SSP submitted within time.
Q. I have dispensed two items on the prescription but have only partially dispensed the third item, how can I claim for the whole prescription?
Where a prescription has gone unclaimed for some time, you may choose to claim for what was dispensed rather than allowing a prescription to reach its 180-day time limit because part of the prescription was not dispensed. Where needed mark an item or part of an item with “not dispensed” and submit your prescription. Some contractors may choose to collect or use patient’s telephone numbers to inform patients about uncollected medicines.
Q. What happens if a price concession is announced after the date that I have sent my claim message to the Pricing Authority for an EPSR2 prescription?
Price concessions, once granted, apply for the whole ‘dispensing month’. For example, a price concession announced on August 30th applies to the entirety of your August ‘prescription bundle’.
Your August prescription bundle is made up of all your paper prescriptions which are sent to the Pricing Authority by the 5th September and all the EPS prescriptions which fall into the August dispensing month (see below). Prescriptions for any one dispensing month are not priced until the Pricing Authority receives both the electronic and paper prescriptions as the FP34C submission document is needed from the paper bundle to calculate the advance payment for the contractor.
How a dispensing month is determined for electronic prescriptions is outlined below:
Further info
If you have queries on this webpage or you require more information please contact it@cpe.org.uk. To share and hear views about digital developments with like-minded pharmacy team members, join the CP Digital email group today.
Return to the Pharmacy IT hub; EPS submission or IT a-z index