Levothyroxine: new prescribing advice if specific product required by patient
The May 2021 MHRA Drug Safety Update contains new prescribing advice for patients who experience symptoms on switching between levothyroxine products.
The advice for healthcare professionals states that:
- generic prescribing of levothyroxine remains appropriate for the majority of patients
- a small proportion of patients treated with levothyroxine report symptoms, often consistent with thyroid dysfunction, when their levothyroxine tablets are changed to a different product
- if a patient reports persistent symptoms when switching between different levothyroxine products, prescribers should consider consistently prescribing a specific levothyroxine product known to be well tolerated by the patient.
- if symptoms or poor control of thyroid function persist (despite adhering to a specific product), prescribers should consider prescribing an oral solution formulation of levothyroxine
Following this advice, community pharmacy teams may expect to receive requests from patients and/or prescribers for a specific brand name or make of levothyroxine to be supplied against a prescription. If a specific levothyroxine product known to be well tolerated by the patient is required, prescribers must ensure the correct product description is selected using their prescribing systems. In EPS, if a specific brand name or supplier of the product is selected, this will appear in the prescription drug name field.
PSNC is aware that some pharmacy contractors have been left out of pocket because prescribers have free-typed product information (such as brand name or supplier) into the dosage instructions field or notes section of electronic prescriptions, and the pharmacy has not been reimbursed for supplying in accordance with the prescribers instructions.
If levothyroxine is prescribed generically, it is reimbursed according to the prices published in Part VIII of the applicable Drug Tariff. However, a prescription requesting levothyroxine by a specific brand name or supplier name is reimbursed according to the NHS list price published in the NHS dictionary of medicines and devices (dm+d). If no price is indicated against the product listing in the dm+d, payment for the non-Part VIII product is based on the dispenser’s endorsement (supplier name, price and pack size).
If an electronic prescription annotated with additional/supplementary product information is received by a pharmacy, it is strongly recommended to have such prescriptions appropriately rewritten/re-issued by the prescriber before dispensing to ensure that it can be accurately priced by the NHSBSA. This is because reimbursement of products ordered using EPS is based on the prescribed product code; any supplementary (free-typed) product information included in the EPS dosage instructions field is not visible to the NHSBSA during prescription pricing. Further information on dealing with EPS product information within the dose area can be found here. The table below shows examples to ensure contractors are correctly reimbursed:
 |
 |
 |
 |
|
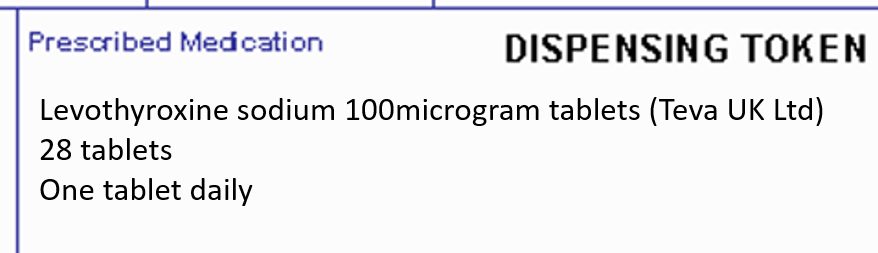
Required manufacturer’s product specified in the drug line field of electronic prescriptions. In this example, contractors will be reimbursed according to Teva UK’s NHS list price for Levothyroxine 100microgram tablets and not as per the basic price listed in Part VIII of the Drug Tariff. |
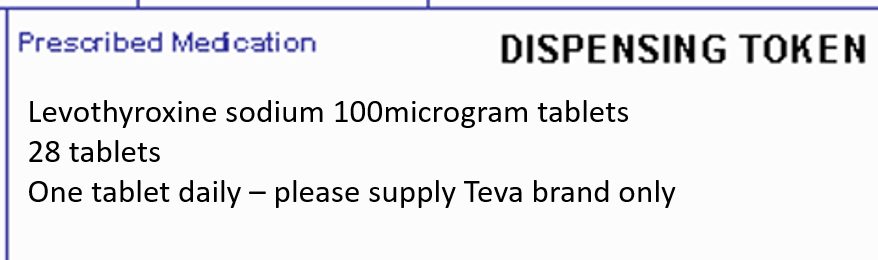
The prescriber has free-typed ‘please supply Teva brand only’ into the dosage instructions field. Product information included in the ‘free text’ fields of the electronic prescription are not extracted by the NHSBSA for reimbursement purposes. Therefore, contractors are reimbursed according to the basic price listed in Part VIII of the Drug Tariff price and NOT as per the NHS list price for the Teva UK product if this was supplied. |
Paper prescriptions with items where prescribers have included supplementary product information (for e.g. brand name or supplier), should be endorsed by the pharmacy as required and submitted for payment within the relevant red separators.
If, for any reason, obtaining a replacement prescription is not practicable and a pharmacy chooses to dispense and endorse a prescription in accordance with supplementary product information, a prescription recheck request can be submitted to the NHSBSA if payment is not reflective of the item supplied. Such recheck requests should be accompanied with suitable evidence for example, a screenshot image or copy of the EPS token showing the prescriber’s indication (supplementary product information) in the dosage area/notes section of the prescription. System suppliers have developed their systems to allow contractors to view and reprint tokens of EPS prescriptions previously submitted for payment.
Dealing with product information within the dose area
Dispensing factsheet: Prescription endorsements
Rechecks requests for prescriptions with additional or supplementary product information