HLP – Introduction and background
Published on: 5th November 2020 | Updated on: 22nd August 2023
The HLP concept was developed in Portsmouth in 2009 with support from the Department of Health (DH), the Director of Public Health and the Local Pharmaceutical Committee following the publication of the 2008 White Paper, Pharmacy in England: building on strengths, delivering the future.
The White Paper described a vision to develop community pharmacies from being suppliers of medicines to become Healthy Living Centres providing self-care advice and treatment for common ailments and healthy lifestyle interventions, in addition to providing the safe supply and use of prescribed medicines.
The HLP framework was launched in September 2010 and Portsmouth HLPs delivered positive interim results. In March 2011, the national pharmacy bodies started working with DH to launch the HLP pathfinder programme, which resulted in an evaluation being published in April 2013. Following this, Public Health England (PHE) adopted the concept and supported the roll out in pharmacies across the country.
In 2016, PHE moved from a commissioner-led to a profession-led, self-assessment process for the attainment of HLP Level 1 status, which included the development of the PHE Quality Criteria. The PHE Quality Criteria underpinned the HLP enablers and set out the criteria that community pharmacies needed to meet to attain HLP Level 1 status.
Following this, NHS England introduced the achievement of HLP Level 1 status, as set out in the PHE Quality Criteria, as a criterion for payment under the Pharmacy Quality Scheme (previously known as the Quality Payments Scheme) for 2017-18.
Collectively, these initiatives introduced greater consistency in the delivery of public health interventions.
What is an HLP?
HLP is an organisational development framework underpinned by three enablers of:
- Workforce Development – A skilled team to pro-actively support and promote behaviour change and improve health and wellbeing, including a qualified Health Champion who has undertaken the Royal Society for Public Health (RSPH) Level 2 Award ‘Understanding Health Improvement’, and a team member who has undertaken leadership training;
- Engagement – Local stakeholder engagement with other health and care professionals (especially general practice), community services, local authorities and members of the public; and
- Environment (Premises Requirements) – Premises that facilitate health promoting interventions with a dedicated health promotion zone.
The adoption of HLPs marked a significant development for community pharmacy and its contribution to health promoting interventions. The HLP framework aims to improve people’s health, help reduce health inequalities and ensures community pharmacy can continue to contribute to the Government’s ambition of putting prevention at the heart of the NHS, as set out in the NHS Long Term Plan.
It provides a mechanism for community pharmacy teams to utilise their local insight and experience in the delivery of high-quality health promoting initiatives. By requiring pharmacy owners to have trained Health Champions on site who pro-actively engage in local community outreach within and outside the pharmacy, HLPs have cemented the idea that every interaction in the pharmacy and the community is an opportunity for a health promoting intervention.
The HLP framework is primarily about adopting a change in culture and ethos within the whole pharmacy team. The HLP framework means community pharmacies can supplement their medicines optimisation role with an enhanced commitment to health promoting interventions in the pharmacy setting and engagement in community outreach activities.
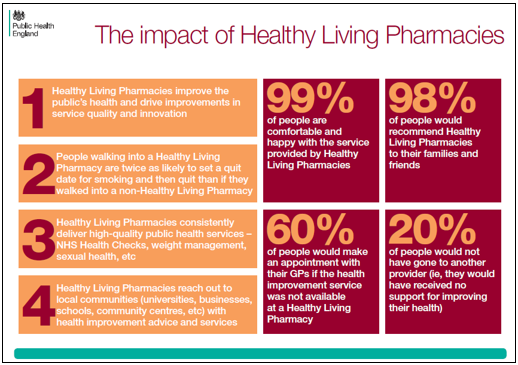
PHE published the below set of infographics in July 2016 to illustrate the role of HLPs in the health and care system.

Evaluation of the HLP pathfinder sites
The evaluation of the HLP pathfinder sites was launched on the 22nd April 2013 and the key findings were:
- early results seen in Portsmouth can be replicated in other areas of the country as the benefits of the scheme were shown not to be dependent on levels of local health need and deprivation;
- the HLP concept was consistent with increased service delivery and improved quality measures and outcomes;
- 21% of people surveyed wouldn’t have done anything if they hadn’t accessed a service or support in the HLP so would have missed out on the benefit of getting advice to improve their health and wellbeing;
- 60% of people surveyed would have otherwise gone to a GP;
- public feedback was positive with 98% saying they would recommend the service to others and 99% were comfortable to receive the service in the pharmacy;
- more people successfully quit smoking in HLPs than non-HLPs or prior to becoming an HLP;
- the number of people who accessed sexual health services and were provided with additional sexual health advice was greater than in non-HLPs;
- the acceptability of community pharmacy as a location for clients to receive an alcohol service and the relatively high levels of activity seen in HLPs compared with non-HLPs showed that HLPs could have an important contribution to this harm reduction service;
- HLPs were effective at delivering increased support for people taking medicines for long term conditions, through both Medicines Use Reviews and the New Medicine Service. Activity was higher for both services in HLPs than non-HLPs or before HLP implementation in all but one site; and
- pharmacies were also positive about the scheme; 70% of the contractors surveyed said it had been worthwhile for their business.
HLP evaluation executive summary
HLP evaluation (full document)
Other evaluations of HLPs
Teeside University – An evaluation of the Tees Healthy Living Pharmacy Pilot Scheme (August 2013)